PROTAC development gains momentum, but clinical performance is poor
Proteolysis targeting chimeras (PROTACs) are heterobifunctional molecules composed of two ligands joined by a linker, designed to degrade proteins by recruiting an E3 ligase to the target, resulting in its subsequent ubiquitylation and degradation by the proteosome. The first concept for a PROTAC was published in 2001, and recently these protein degraders have gained rapid momentum as a promising novel modality. Due to the catalytic mechanism of action, PROTACs are stipulated to have clinical advantages in indications where degrading the whole protein is more therapeutically beneficial, where covalent inhibitors are insufficient to fully block the oncogenic functions of the target or may not be selective enough.
Other advantages include that PROTACs are pharmaceutically active in picomolar doses due to the ‘reusable’ nature of the modality, as the PROTAC itself doesn’t get degraded and is instead free to catalyze further degradation of the target. This makes early R&D less risky, as many lead compounds are discontinued due to inadequate pharmacokinetic profiles and require excessively high dosages to be pharmaceutically active. Additionally, PROTACs are stipulated to be more selective than conventional small molecule inhibitors due to having fewer requirements to satisfy for binding to the target, because the active domain of the heterobifunctional molecule is only required to bind to the target and does not need to elicit any changes in target function, unlike conventional small molecule inhibitors that have to satisfy a demanding set of requirements such as selectively binding to a domain of the target to elicit a change in target function, which can be a challenging part of the drug development.
By this same virtue, PROTACs are able to degrade previously undruggable targets, which provides a major competitive advantage for this modality if shown to be true. Moreover, PROTACs may allow for tissue-specific target degradation, contingent on tissue-specific expression of E3 ligases for which the PROTAC can leverage. However, the expendability of certain E3 ligases raises questions regarding whether cancer cells can lose dependence on the E3 ligase and consequently become resistant to the PROTAC.
According to the GlobalData Pharma Intelligence Center, there are currently 71 PROTACs in development in the oncology pipeline by non-academic developers, mostly clustering in the preclinical and discovery phases, with only 14 agents in clinical stages. Non-small cell lung cancer leads as the indication with the highest number of PROTACs in the pipeline, currently sitting at 11 preclinical candidates. However, metastatic castration-resistant prostate cancer (mCRPC) has the most mature pipeline with two out of a total of eight PROTACs in development for mCRPC in Phase II trials. Both degraders, ARV-110 (bavdegalutamide) and ARV-766, are being developed by Arvinas. GlobalData’s analyst consensus forecast database estimates peak annual sales for ARV-110 of $325 million in 2028.
In 2021, Pfizer entered the PROTAC space by signing a deal with Arvinas worth a total of $1 billion: $650 million upfront and $350 million invested into the commercialization and development of Arvinas’s estrogen receptor (ER) PROTAC, ARV-471. Unfortunately, ARV-471 was recently reported to yield a lackluster 3% response rate in 71 heavily pretreated ER-positive/HER2-negative breast cancer patients in the VERITAC Phase II single-arm trial investigating ARV-471 in combination with Pfizer’s CDK4/6 inhibitor Ibrance (palbociclib). All patients had received CDK4/6 inhibitors, and 79% had received AstraZeneca’s ER non-PROTAC degrader Faslodex (fulvestrant). Among 44 patients with measurable disease, two had confirmed partial responses. The primary endpoint was clinical benefit rate, which came in at a mediocre 38%; Faslodex had demonstrated a clinical benefit rate of 54.9% in the second-line setting in the FINDER1 randomized Phase II trial. Surprisingly, ARV-471 has progressed to Phase III to be evaluated in a less heavily pretreated population where all patients have received CDK4/6 inhibitors, but unlike the Phase II, patients who have received Faslodex or chemotherapy for advanced disease will be excluded. Faslodex will be administered in the control arm of the Phase III study, allowing for direct comparison between the two ER degraders.
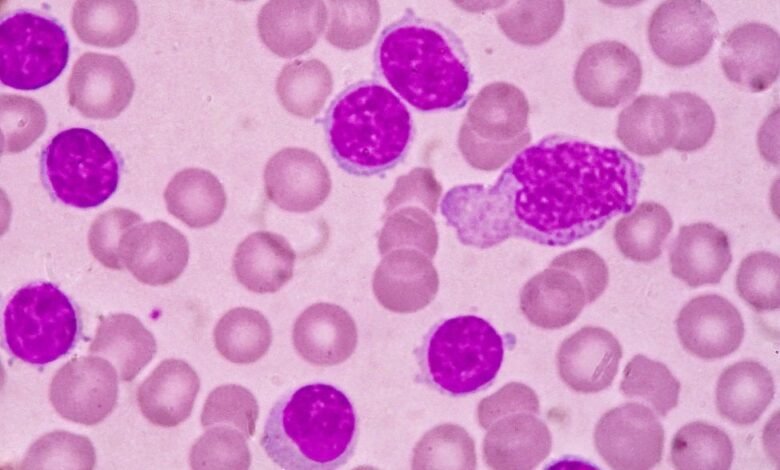
Despite PROTACs putatively possessing the advantage of potentially targeting previously undruggable targets, the most common disclosed targets in the PROTAC pipeline are the androgen receptor (AR) (nine PROTACs) and Bruton’s tyrosine kinase (BTK) (seven PROTACs). The AR and BTK are both very well-established targets, in mCRPC and B-cell malignancies, respectively. AR and BTK being the most popular disclosed PROTAC targets may be reflective of risk-mitigation strategies employed whereby PROTACs are developed to degrade well-established targets rather than targeting previously undruggable targets, as it is unclear as to whether degradation of these targets can produce a therapeutically desirable effect in the clinic. Importantly, PROTACs targeting BTK may possess a competitive advantage over conventional BTK small molecule inhibitors that are more susceptible to secondary resistance due to well-characterised hotspot mutations that cause patients to lose responsiveness to the therapy. PROTACs are less susceptible to hotspot mutations because lower binding affinity doesn’t abrogate the ability for the PROTAC to degrade the target, whereas conventional inhibitors lose efficacy due to decreased binding affinity.
In chronic lymphocytic leukemia (CLL), it is common for patients to cycle through several different BTK inhibitors (BTKis) due to the development of BTK mutations. Moreover, off-target effects from conventional BTKis result in a suboptimal safety profile, which the enhanced selectivity of PROTACs can help mitigate. However, on-target adverse events are also common with BTKis as they inhibit B-cell immune responses, which can result in serious infections. Indeed, it is also well known that the toxicity profiles of BTKis are closely linked to their selectivity profiles; AstraZeneca’s Calquence (acalabrutinib), a highly selective second-generation BTKi, has demonstrated noninferiority to a first-generation BTKi, Johnson & Johnson’s Imbruvica (ibrutinib), while demonstrating a significantly more tolerable safety profile with lower instances of cardiac toxicity (atrial fibrillations: 9.4% with Calquence, 16% with Imbruvica, NCT02477696). This warrants further investigation into whether PROTACs can leverage the enhanced selectivity of the modality without inducing unacceptable levels of on-target adverse events.
Source link
#PROTAC #development #gains #momentum #clinical #performance #poor