What’s missing from the NHS Long Term Workforce Plan

Back in the days of the Healthcare Commission’s annual health check, policies and procedures were central to quality. It certainly felt like that when the mental health clinical governance team I was in spent hours ensuring practice followed policy. I also learnt the value of staff involvement in policy and its impact on retention. So, when I spotted the inclusion of this often overlooked aspect of retention in an evidence synthesis, I wanted to read on.
As part of the Health Foundation funded Efficiency Research programme, researchers from the University of Sheffield reviewed literature from 2004-2020 (Long, et al, 2023) to explore staff retention in mental health services. By chance, I read this synthesis within the same week as the NHS Long Term Workforce Plan (NHSE, 2023). I wondered if the authors of the Plan had read this review and concluded they hadn’t. The synthesis underlined what was missing from the Plan.

I wondered if the authors of the NHS Long Term Workforce Plan had read this synthesis on retention. I decided they hadn’t.
Methods
The researchers conducted a realist synthesis. A method aiming to develop theories explaining why interventions work (or don’t), how they work and in what contexts. The researchers undertook the review in 3 ‘hybrid’ phases (Rycroft-Malone, et al 2012), combining traditional review methods with people’s views, including:
- Exploratory scoping of literature alongside workshops, from which they developed preliminary theories;
- Searches and data extraction;
- Analysis of data, refining theories and development of a logic model.
Three key elements of richness, relevance and rigour were considered. Diverse stakeholders, including staff and service users, helped test and refine the theories.
Results
The first phase of the review generated 6 preliminary theories on effective retention for further exploration. The formal search in the second phase generated data that was used to identify key factors and issues against each theory. Analysis of the data showed that themes from across the 6 theories interconnected and overlapped. As a result, in phase three the team integrated and refined the 6 theories into 3 key drivers, which represented a whole systems perspective on effective retention, starting with organisational culture and consisting of:
- Workload and quality of care
- If staff experience high workload,
- then they will feel they have to deliver lower quality care to manage time demands;
- Staff investment
- If organisations invest in training, development and supervision,
- then staff will feel more confident to deliver higher quality care;
- Staff input
- If staff shape the development of policies and practice,
- then they will feel valued and supported to work autonomously.
Analysis indicated that these drivers all impact on wellbeing, sense of connectedness to an organisation and ultimately job satisfaction. To show the relationships between these theories the team created an overarching logic model.
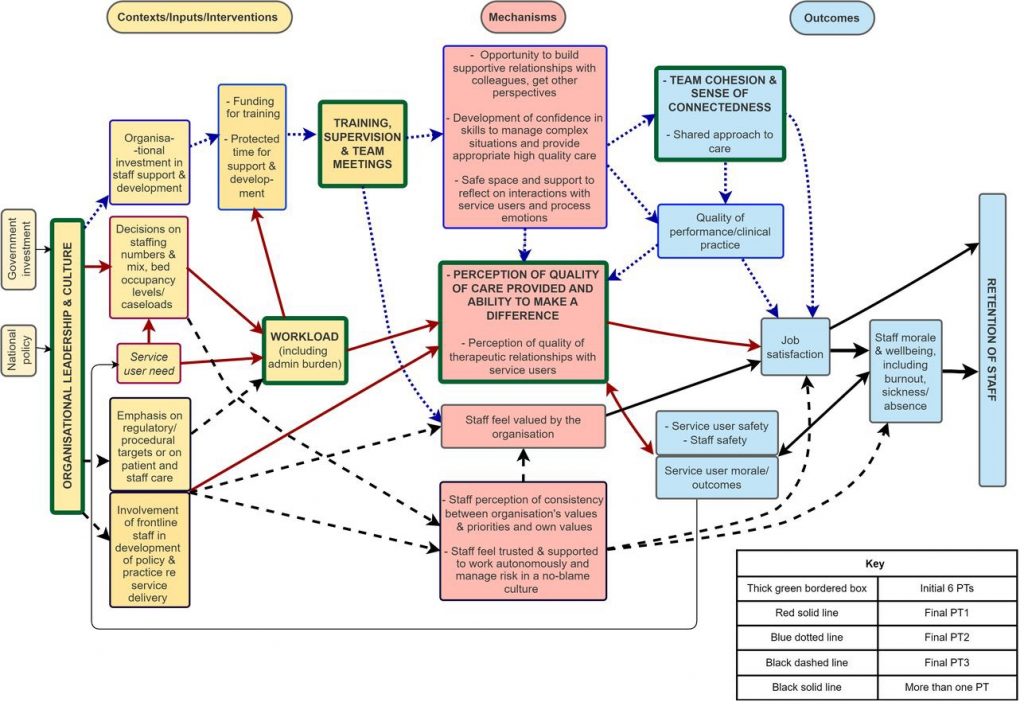
Figure 1 The logic model of factors affecting the retention of mental health staff. View full-sized figure.
What’s valuable about this review, is not only that it enhances our understanding of retention, but it generates a whole systems perspective. A perspective unfortunately missing from the Long-Term Workforce Plan.

The 3 key drivers of effective staff retention: workload & quality of care, investment and involvement, stem from organisational culture and demand a whole systems perspective.
Conclusions
The Workforce Plan picks up some of the factors identified by the review, for example training. However, the focus is on growing numbers of staff. The importance of investing in people emphasised in the review is less apparent. The Plan acknowledges the significant workload issues for mental health settings, but fails to acknowledge the interconnectedness with quality of care. The third factor for successful retention: staff input in policy development, doesn’t even get a mention. The nearest the Plan gets is a section entitled ‘we have a voice that counts’.
The authors of the Plan seem to have missed the key point this review underlines, simply recruiting more staff is unlikely to solve the issues. We need to keep them. This central point is best summed up in realist terms:
- If workforce planning enabled a whole systems approach to tackling retention,
- Then quality of care would increase and staff job satisfaction improve,
- Leading to…. more staff staying.

Simply recruiting more staff is unlikely to solve the issues. We need to keep them.
Strengths and limitations
The real strength of this review is not simply what it tells us about retention in mental health services, but what it offers us as a case study for other UK health settings. It may not ‘prove’ something, but we can learn something (Flyvbjerg, 2006). As the NHS Workforce Plan acknowledges, mental health services have higher turnover and more vacancies than other staff groups. Staff face particular issues from the nature of care, such as monitoring risk of suicide and experience reportedly higher emotional exhaustion than colleagues in emergency settings (O’Connor, et al, 2018). Moreover, even though the bulk of the reviewed studies were from inpatient settings, the involvement of diverse staff and service users in developing the theories helps to ensure that the findings have wider applicability.
One of the main limitations acknowledged by the researchers is their focus on “interpretation rather than ensuring the most comprehensive identification of information” (Long et al, 2023). This means that the review may not have picked up all potential sources. The emphasis on the need to interpret may have also contributed to a seeming lack of emphasis on appraisal, at least in the article. The researchers state that “Judgements on study quality were deferred until later stages of analysis”. Unfortunately, no further details are provided in the article on how study quality was judged and the reader is left wondering what impact deferring had on the conclusions that were reached.
The real strength of this review is not simply what it tells us about retention in mental health services, but what it offers us as a case study that may not ‘prove’ something, but where we can learn something.
Implications for practice
This synthesis generates implications for several groups. Firstly, for policy makers, highlighting the need to retain, not simply recruit staff. Also, for retention to be approached using a whole system perspective that tackles the interconnecting issues. The interconnectedness of the factors affecting retention is equally important for service providers. The review underlines the need to start with organisational culture and employ strategies that recognise:
- The interconnectedness of workload and quality of care
- The need to invest in training and development
- The importance of staff autonomy through involvement in how quality care is articulated and practised (often forgotten).
Finally, this review offers an implication for funders of health and social care research, especially those operating in the landscape of complex interventions. If we are to play a role in improving the evidence base, reducing uncertainties and improving care (HRA, 2023), then we need to support syntheses of the evidence that help us understand not just what works, but also how.

The implications are not only for service providers, or policy makers, but also research funders who should support syntheses that help us understand what works and how.
Statement of interests
Justine Karpusheff is Assistant Director of Research at The Health Foundation. The Health Foundation funded this study as part of the Efficiency Research Programme.
Links
Primary paper
Long J, Ohlsen S, Senek M, Booth A, Which S, Wood E. (2023) Realist synthesis of factors affecting retention of staff in UK adult mental health services. BMJ Open, 13(5) 2023. Available at: https://bmjopen.bmj.com/content/13/5/e070953#DC1
Other references
NHSE (2023) NHS Long-term workforce plan. June 2023. Available at: https://www.england.nhs.uk/wp-content/uploads/2023/06/nhs-long-term-workforce-plan-v1.2.pdf
Rycroft-Malone J, McCormack B, Hutchinson A M. et al (2012) Realist synthesis: illustrating the method for implementation research. Implementation Science, 7(33) 2012. Available at: https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-7-33
Flyvbjerg B. (2006) Five Misunderstandings about case-study research. Qualitative Inquiry, 12(2) 2006. [abstract]
O’Connor K, Muller Neff D, Pitman S. (2018) Burnout in mental health professionals: a systematic review and meta-analysis of prevalence and determinants. European Psychiatry, 53. Available at: https://www.cambridge.org/core/journals/european-psychiatry/article/burnout-in-mental-health-professionals-a-systematic-review-and-metaanalysis-of-prevalence-and-determinants/8DE6B29F7AD65E2442726CA8D1F7F876
Health Research Authority (2023) UK Policy Framework for Health and Social Care. Available at: https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/uk-policy-framework-health-social-care-research/uk-policy-framework-health-and-social-care-research/
Source link
#Whats #missing #NHS #Long #Term #Workforce #Plan

