Party with a Purpose Honors Neuroblastoma Researchers
Neuroblastoma, a rare cancer that occurs primarily in children, is a scientific paradox, said pediatric oncologist John M. Maris, MD, of Children’s Hospital of Philadelphia (CHOP).
“On one hand, a fairly high percentage of these tumors go away on their own, without any therapy. On the other hand, in about half of patients, it is one of the most aggressive childhood cancers,” Maris said.
In his over 30-year career with CHOP, Maris has helped develop innovative treatments for neuroblastoma that have helped increase survival rates for high-risk neuroblastoma patients from about 30% to 50%. As co-head of the Pediatric Cancer Dream Team and the Giulio D’Angio Chair in Neuroblastoma Research, he leads research aimed at improving those survival rates and designing treatments that might take less of a toll on young patients.
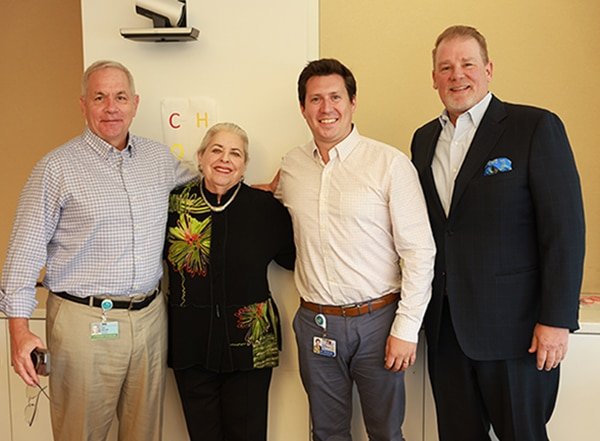
This year, in recognition of his pioneering research on neuroblastoma and other childhood cancers, Maris will receive the Scientific Achievement Award from Party with a Purpose, an annual event that raises funds for cancer research. As part of the unique mission of Party with a Purpose, Maris selected Timothy Spear, MD, PhD, a pediatric hematology/oncology fellow at CHOP, to receive the Early-Career Investigator research grant. These awards are given in conjunction with the Friends of the American Association for Cancer Research Foundation. This year’s Humanitarian Award will honor Beverly Fassler Goldberg, longtime president of the foundation, for her tireless efforts in raising funds for cancer research.
Maris, Spear, and Goldberg will be honored at a gala in Philadelphia on October 29. Maris and Spear discussed their work on neuroblastoma with Cancer Research Catalyst.
What drew you to pediatric research?
Maris: I came to this campus almost 40 years ago to the day. As a research technician in a Penn lab I had the opportunity work on a neuroblastoma project with Drs. Audrey Evans and Dan (Giulio) D’Angio, who were leaders in the department of oncology at the Children’s Hospital. So, for the next two years, I had a pretty deep dive into not only trying to understand childhood cancer, but also watching these amazing physicians interact with patients and their families. It just blew me away. When I went to medical school, I focused on pediatrics and ultimately became a pediatric oncologist.
Spear: When I began my combined MD/PhD program, I chose a cancer immunology lab that was focused on liver cancer and hepatitis C virus infection. At that time, my clinical interests were adult gastroenterology and liver transplantation, but when it came time to do my clinical clerkship as a third-year medical student, I fell in love with pediatrics and switched my entire fourth year to focus on pediatric subspecialties. One of my mentors in medical school was a pediatric oncologist. I looked up to him a lot, and he served as a beacon for me in refining what my clinical and research interests were.
What led to your current focus on neuroblastoma?
Maris: As we try to discern whether a patient with neuroblastoma has a high-risk or a low-risk case, we can stare at it in a microscope, and it looks pretty much the same whether you have one form or the other. We have focused on the genetics that define how neuroblastoma behaves and can be leveraged therapeutically. That’s what fascinates us from an intellectual standpoint and provides our motivation for improving patient outcomes through precision therapies.
Yes, there has been progress against neuroblastoma; unfortunately, the way we’ve made that progress is by quadrupling the amount of very noxious therapy that children get. As we’ve been able to improve the way we support patients in the ICUs, we’ve pushed the boundaries of what kids can tolerate. That’s cured a few more patients, but with a lot of morbidity. We’ve clearly reached a plateau of what we can do with chemotherapy and radiation therapy. To move forward, we have developed precision medicines and immunotherapies that are in various stages of clinical trials. These treatments give us a lot of hope … but there’s still a lot of work to do.
Spear: Neuroblastoma is an interesting disease from a biology standpoint, and in how it evolves in patients. And with a cure rate of just under a coin flip for individuals with high-risk disease, there’s a large gap in what we need to do. For a young investigator, that’s a large window to try to make progress. Even as a fellow, I’m mentored to be a primary oncologist for a number of patients, and a high-risk neuroblastoma patient that I care for just relapsed. It’s those patient experiences that motivate me to make much-needed progress in the lab. The kids are always the inspiration for us. While they will eventually provide the answers for how we create next-generation personalized treatments, they’re also the reason we’re here and keep showing up to work.
How do your research interests intersect, and what is the current focus of your research?
Maris: Our neuroblastoma team at CHOP is focused on translating basic and clinical research into improved therapies for patients. One of these potential areas is cancer vaccines. In childhood cancers, therapeutic vaccines have the potential to cure some cases and prevent relapses in others. Tim is testing some novel strategies on how to not just make a neuroblastoma vaccine in general, but to make a neuroblastoma vaccine specifically for each individual patient based on their own tumors genetic make-up. This personalized approach is especially feasible in the relatively rare types of cancer, such as neuroblastoma.
Spear: We work with patient biopsies to identify the unique genetic or protein signature that can help us design a vaccine that would make patients’ immune systems responsive to their cancer. We’re developing some unique mouse models that have, essentially, a patient’s immune cells circulating in the mouse with the patient’s matched tumor growing on the side of the mouse. We plan on testing the ability of a personalized vaccine to stimulate the patient’s immune system that’s engrafted in that mouse to attack and eliminate the cancer. I think it’s a really unique tool that will have quite a bit of impact if and when it works.
How do financial awards like the Party with a Purpose award help facilitate your work?
Maris: When Tim came to the lab, we had this idea, and we wrote a grant together seeking funding from the National Institutes of Health. It takes at least nine months, but sometimes years, from the time you write a grant to when you actually get money for the project. We were confident about this project, but you never know.
Tim’s been able to make significant progress, and we planned to apply for some additional funding so that we could afford to hire a technician to work with him. Once we learned about the Party with a Purpose grant, we went ahead and hired Elizabeth, who is in the lab now; she’s been with us about two weeks. To know that money is coming gives us the confidence to move forward with hiring. And that’s how you move science forward … with people.
Spear: Philanthropic awards like this are invaluable to a young investigator. As an early-career researcher applying for grants, you often need publications or previous funding to convince someone that you’re worthy enough to fund. That process can take a very long time. With philanthropy like this, that money is immediately usable and accessible. Hiring an extra set of hands in the lab is just going to accelerate the progress of our project.
What does mentorship mean to each of you?
Maris: I benefited tremendously from mentors who really cared … not just that we got the work done, but how our careers developed and how we would make an impact. I now spend a considerable amount of time mentoring. There are holistic reasons to do that, there are academic reasons to do that … but another major reason is that the work that I’m able to achieve in my career is not going to finish the job. It would be great if it did, but I don’t have that illusion. Guiding the next generation of superstars to really pay this forward and become the future mentors is crucial. Tim has all the markings of someone who will do this.
Spear: Mentorship is everything for a trainee. You need to have people who support you within the lab but can also instill confidence in you that your ideas are valid; give you the independence to try new things; give you room to fail; and allow you to work through failures to learn from them and really succeed. John has given me a lot of latitude to craft my own ideas within the framework of the project that we’ve come up with.
What is the next frontier in pediatric cancer research? How can outcomes be improved for the cancers that don’t yet have cures or good treatments?
Maris: The phrase that has stuck with me my entire career, which was coined by Dan D’Angio, is “Cure is not enough.” We have to cure with quality. We have to intercept relapse early, before it occurs. And we need to cure more patients without harming them. We’ve mapped the landscape, but the challenge has been turning that into more effective therapies. That is the frontier: having curative, less toxic therapy for every patient, so that children won’t be burdened with lifelong side effects.
Spear: The journey to cure has many ups and downs. Many of the up-front regimens that we use to try to cure have devastating side effects and some can be debilitating. To me, the next frontier is threading that needle of producing lasting cures while minimizing the side effects.
Source link
#Party #Purpose #Honors #Neuroblastoma #Researchers



