Editors’ Picks: June Highlights From the AACR Journals
As we head into summer, enjoy this month’s selection of studies spotlighted by the editors of the 10 AACR journals. Highlights include the results of three clinical trials, a genomic analysis of Hodgkin lymphoma evolution, a study of the regional variations in breast cancer in sub-Saharan Africa, a mechanism of T-cell exclusion from tumors, and more.
The abstracts of this month’s highlighted studies are included below, and the full text of each article will be freely available for a limited time.
Journal: Blood Cancer Discovery
The rarity of malignant Hodgkin and Reed Sternberg (HRS) cells in classic Hodgkin lymphoma (cHL) limits the ability to study the genomics of cHL. To circumvent this, our group has previously optimized fluorescence-activated cell sorting to purify HRS cells. Using this approach, we now report the whole-genome sequencing landscape of HRS cells and reconstruct the chronology and likely etiology of pathogenic events leading to cHL. We identified alterations in driver genes not previously described in cHL, APOBEC mutational activity, and the presence of complex structural variants including chromothripsis. We found that high ploidy in cHL is often acquired through multiple, independent chromosomal gains events including whole-genome duplication. Evolutionary timing analyses revealed that structural variants enriched for RAG motifs, driver mutations in B2M, BCL7A, GNA13, and PTPN1, and the onset of AID-driven mutagenesis usually preceded large chromosomal gains. This study provides a temporal reconstruction of cHL pathogenesis.
Significance: Previous studies in cHL were limited to coding sequences and therefore not able to comprehensively decipher the tumor complexity. Here, leveraging cHL whole-genome characterization, we identify driver events and reconstruct the tumor evolution, finding that structural variants, driver mutations, and AID mutagenesis precede chromosomal gains.
This study was highlighted in the current issue.
Journal: Cancer Discovery
Late-stage Metastatic Melanoma Emerges Through a Diversity of Evolutionary Pathways
Understanding the evolutionary pathways to metastasis and resistance to immune-checkpoint inhibitors (ICI) in melanoma is critical for improving outcomes. Here, we present the most comprehensive intrapatient metastatic melanoma dataset assembled to date as part of the Posthumous Evaluation of Advanced Cancer Environment (PEACE) research autopsy program, including 222 exome sequencing, 493 panel-sequenced, 161 RNA sequencing, and 22 single-cell whole-genome sequencing samples from 14 ICI-treated patients. We observed frequent whole-genome doubling and widespread loss of heterozygosity, often involving antigen-presentation machinery. We found KIT extrachromosomal DNA may have contributed to the lack of response to KIT inhibitors of a KIT-driven melanoma. At the lesion-level, MYC amplifications were enriched in ICI nonresponders. Single-cell sequencing revealed polyclonal seeding of metastases originating from clones with different ploidy in one patient. Finally, we observed that brain metastases that diverged early in molecular evolution emerge late in disease. Overall, our study illustrates the diverse evolutionary landscape of advanced melanoma.
Significance: Despite treatment advances, melanoma remains a deadly disease at stage IV. Through research autopsy and dense sampling of metastases combined with extensive multiomic profiling, our study elucidates the many mechanisms that melanomas use to evade treatment and the immune system, whether through mutations, widespread copy-number alterations, or extrachromosomal DNA.
This study was highlighted and featured on the cover of the June issue. A related commentary is available here.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Background: Routine human papillomavirus (HPV) vaccination is recommended for young adults, yet many young gay, bisexual, and other men who have sex with men (YGBMSM) remain unvaccinated. We report the efficacy of Outsmart HPV, a web-based HPV vaccination intervention for YGBMSM.
Methods: From 2019 to 2021, we recruited YGBMSM in the United States who were ages 18–25 and unvaccinated against HPV (n = 1,227). Participants were randomized to receive either: (i) Outsmart HPV content online and monthly interactive text reminders (interactive group); (ii) Outsmart HPV content online and monthly unidirectional text reminders (unidirectional group); or (iii) standard information online about HPV vaccine (control group). Regression models compared study groups on HPV vaccination outcomes.
Results: Overall, 33% of participants reported initiating the HPV vaccine series and 7% reported series completion. Initiation was more common among participants in the interactive group compared with the control group [odds ratio (OR) = 1.47, 98.3% confidence interval (CI): 1.03–2.11]. Completion was more common among participants in both the interactive group (OR = 3.70, 98.3% CI: 1.75–7.83) and unidirectional group (OR = 2.26, 98.3% CI: 1.02–5.00) compared with the control group. Participants who received Outsmart HPV content reported higher levels of satisfaction with online content compared with the control group.
Conclusions: Outsmart HPV is an efficacious and acceptable HPV vaccination intervention for YGBMSM. Future efforts are needed to determine how to optimize the intervention and disseminate it to settings that provide services to YGBMSM.
Impact: Outsmart HPV is a promising tool for increasing HPV vaccination among YGBMSM with the potential for wide dissemination.
This study was highlighted in the June issue.
Journal: Cancer Immunology Research
The low overall survival rates of patients with breast cancer in sub-Saharan Africa (SSA) are driven by regionally differing tumor biology, advanced tumor stages at diagnosis, and limited access to therapy. However, it is not known whether regional differences in the composition of the tumor microenvironment (TME) exist and affect patients’ prognosis. In this international, multicenter cohort study, 1,237 formalin-fixed, paraffin-embedded breast cancer samples, including samples of the “African Breast Cancer-Disparities in Outcomes (ABC-DO) Study,” were analyzed. The immune cell phenotypes, their spatial distribution in the TME, and immune escape mechanisms of breast cancer samples from SSA and Germany (n = 117) were investigated using histomorphology, conventional and multiplex IHC, and RNA expression analysis. The data revealed no regional differences in the number of tumor-infiltrating lymphocytes (TIL) in the 1,237 SSA breast cancer samples, while the distribution of TILs in different breast cancer IHC subtypes showed regional diversity, particularly when compared with German samples. Higher TIL densities were associated with better survival in the SSA cohort (n = 400), but regional differences concerning the predictive value of TILs existed. High numbers of CD163+ macrophages and CD3+CD8+ T cells accompanied by reduced cytotoxicity, altered IL10 and IFNγ levels and downregulation of MHC class I components were predominantly detected in breast cancer samples from Western SSA. Features of nonimmunogenic breast cancer phenotypes were associated with reduced patient survival (n = 131). We therefore conclude that regional diversity in the distribution of breast cancer subtypes, TME composition, and immune escape mechanisms should be considered for therapy decisions in SSA and the design of personalized therapies.
A related commentary on this study is available here.
Journal: Cancer Prevention Research
Suberoylanilide hydroxamic acid (SAHA) is a histone deacetylase (HDAC) inhibitor with anticancer effects via epigenetic and non-epigenetic mechanisms. The role of SAHA in metabolic rewiring and epigenomic reprogramming to inhibit pro-tumorigenic cascades in lung cancer remains unknown. In this study, we aimed to investigate the regulation of mitochondrial metabolism, DNA methylome reprogramming, and transcriptomic gene expression by SAHA in lipopolysaccharide (LPS)-induced inflammatory model of lung epithelial BEAS-2B cells. LC/MS was used for metabolomic analysis, while next-generation sequencing was done to study epigenetic changes. The metabolomic study reveals that SAHA treatment significantly regulated methionine, glutathione, and nicotinamide metabolism with alteration of the metabolite levels of methionine, S-adenosylmethionine, S-adenosylhomocysteine, glutathione, nicotinamide, 1-methylnicotinamide, and nicotinamide adenine dinucleotide in BEAS-2B cells. Epigenomic CpG methyl-seq shows SAHA revoked a list of differentially methylated regions in the promoter region of the genes, such as HDAC11, miR4509–1, and miR3191. Transcriptomic RNA sequencing (RNA-seq) reveals SAHA abrogated LPS-induced differentially expressed genes encoding proinflammatory cytokines, including interleukin 1α (IL1α), IL1β, IL2, IL6, IL24, and IL32. Integrative analysis of DNA methylome-RNA transcriptome displays a list of genes, of which CpG methylation correlated with changes in gene expression. qPCR validation of transcriptomic RNA-seq data shows that SAHA treatment significantly reduced the LPS-induced mRNA levels of IL1β, IL6, DNA methyltransferase 1 (DNMT1), and DNMT3A in BEAS-2B cells. Altogether, SAHA treatment alters the mitochondrial metabolism, epigenetic CpG methylation, and transcriptomic gene expression to inhibit LPS-induced inflammatory responses in lung epithelial cells, which may provide novel molecular targets to inhibit the inflammation component of lung carcinogenesis.
Prevention Relevance: Inflammation increases the risk of lung cancer and blocking inflammation could reduce the incidence of lung cancer. Herein, we demonstrate that histone deacetylase inhibitor suberoylanilide hydroxamic acid regulates metabolic rewiring and epigenetic reprogramming to attenuate lipopolysaccharide-driven inflammation in lung epithelial cells.
This study was featured on the cover of the June issue.
Journal: Cancer Research (June 1 issue)
ANO1 Reprograms Cholesterol Metabolism and the Tumor Microenvironment to Promote Cancer Metastasis
Tumor metastasis is a complex process. A better understanding of the mechanistic underpinnings of the metastatic cascade could uncover approaches to better prevent and target metastases. Here, we integrated transcriptomic profiling in primary esophageal squamous cell carcinoma (ESCC) and matched lymph node metastatic tissues and genome-wide CRISPR/Cas9 functional screening to identify the key drivers of cancer metastasis. Anoctamin 1 (ANO1) expression was found to be elevated in primary tumors and further increased in metastatic tissues. High expression of ANO1 was associated with poor patient survival, and ANO1 overexpression promoted cancer invasion and metastasis. Mechanistically, ANO1 inactivated the LXR pathway and increased intracellular cholesterol accumulation by interacting with JUN to repress the transcription of cholesterol hydroxylase, CYP27A1. In a paracrine manner, IL1β secreted from ANO1-expressing ESCC cancer cells activated NF-κB signaling in fibroblasts to stimulate production of the chemokine CCL1, which in turn enhanced invasion of ESCC cancer cells. Furthermore, molecular docking and in silico screening of 1,500,000 small molecules identified K786–4469 as a lead compound that targeted ANO1 and suppressed cancer metastasis in vitro and in vivo. Overall, these findings uncover a noncanonical function of ANO1 in regulating cholesterol metabolism and fibroblast function, revealing ANO1 as a potential prognostic biomarker and therapeutic target for metastatic ESCC.
Significance: Metastatic cancer cells upregulate ANO1 to activate cell-intrinsic and -extrinsic mechanisms that alter cholesterol metabolism and stimulate fibroblasts, which can be targeted with ANO1 inhibitors to inhibit metastatic growth.
A related commentary on this study is available here.
Journal: Cancer Research (June 15 issue)
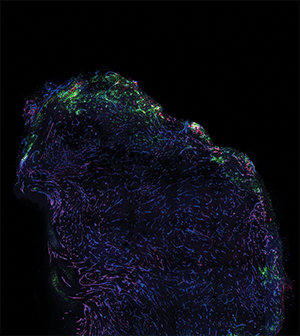
T-cell position in the tumor microenvironment determines the probability of target encounter and tumor killing. CD8+ T-cell exclusion from the tumor parenchyma is associated with poor response to immunotherapy, and yet the biology that underpins this distinct pattern remains unclear. Here we show that the vascular destabilizing factor angiopoietin-2 (ANGPT2) causes compromised vascular integrity in the tumor periphery, leading to impaired T-cell infiltration to the tumor core. The spatial regulation of ANGPT2 in whole tumor cross-sections was analyzed in conjunction with T-cell distribution, vascular integrity, and response to immunotherapy in syngeneic murine melanoma models. T-cell exclusion was associated with ANGPT2 upregulation and elevated vascular leakage at the periphery of human and murine melanomas. Both pharmacologic and genetic blockade of ANGPT2 promoted CD8+ T-cell infiltration into the tumor core, exerting antitumor effects. Importantly, the reversal of T-cell exclusion following ANGPT2 blockade not only enhanced response to anti-PD-1 immune checkpoint blockade therapy in immunogenic, therapy-responsive mouse melanomas, but it also rendered nonresponsive tumors susceptible to immunotherapy. Therapeutic response after ANGPT2 blockade, driven by improved CD8+ T-cell infiltration to the tumor core, coincided with spatial TIE2 signaling activation and increased vascular integrity at the tumor periphery where endothelial expression of adhesion molecules was reduced. These data highlight ANGPT2/TIE2 signaling as a key mediator of T-cell exclusion and a promising target to potentiate immune checkpoint blockade efficacy in melanoma.
Significance: ANGPT2 limits the efficacy of immunotherapy by inducing vascular destabilization at the tumor periphery to promote T-cell exclusion.
This study was featured on the cover of the June 15 issue.
Journal: Clinical Cancer Research (June 1 issue)
Purpose: Isocitrate dehydrogenase 1 (IDH1) mutations occur in 5% to 10% of patients with acute myeloid leukemia (AML). Ivosidenib is an IDH1 inhibitor, approved for use in patients with IDH1-mutated AML.
Patients and Methods: We conducted a multicenter, phase I trial of maintenance ivosidenib following allogeneic hematopoietic cell transplantation (HCT) in patients with IDH1-mutated AML. Ivosidenib was initiated between days 30 and 90 following HCT and continued for up to 12 28-day cycles. The first dose level was 500 mg daily, with level reduction to 250 mg daily, if needed, in a 3 × 3 de-escalation design. Ten additional patients would then receive the MTD or recommended phase 2 dose (RP2D). The primary endpoint was establishing the MTD or RP2D of ivosidenib.
Results: Eighteen patients were enrolled, of whom 16 initiated post-HCT ivosidenib. One dose-limiting toxicity, grade(g) 3 QTc prolongation, was observed. The RP2D was established at 500 mg daily. Attributable g≥3 adverse events were uncommon, with the most common being QTc prolongation in 2 patients. Eight patients discontinued maintenance, with only one due to adverse event. Six-month cumulative incidence (CI) of gII-IV aGVHD was 6.3%, and 2-year CI of all cGVHD was 63%. Two-year CI of relapse and nonrelapse mortality (NRM) were 19% and 0%, respectively. Two-year progression-free (PFS) was 81%, and 2-year overall survival (OS) was 88%.
Conclusions: Ivosidenib is safe and well-tolerated as maintenance therapy following HCT. Cumulative incidence of relapse and NRM, as well as estimations of PFS and OS, were promising in this phase I study.
This article was highlighted in the June 1 issue.
Journal: Clinical Cancer Research (June 15 issue)
Purpose: Eganelisib (IPI-549) is a first-in-class, orally administered, highly selective PI3Kγ inhibitor with antitumor activity alone and in combination with programmed cell death protein 1/ligand 1 (PD-1/PD-L1) inhibitors in preclinical studies. This phase 1/1b first-in-human, MAcrophage Reprogramming in Immuno-Oncology-1 (NCT02637531) study evaluated the safety and tolerability of once-daily eganelisib as monotherapy and in combination with nivolumab in patients with solid tumors.
Patients and Methods: Dose-escalation cohorts received eganelisib 10–60 mg as monotherapy (n = 39) and 20–40 mg when combined with nivolumab (n = 180). Primary endpoints included incidence of dose-limiting toxicities (DLT) and adverse events (AE).
Results: The most common treatment-related grade ≥3 toxicities with monotherapy were increased alanine aminotransferase (ALT; 18%), aspartate aminotransferase (AST; 18%), and alkaline phosphatase (5%). No DLTs occurred in the first 28 days; however, toxicities meeting DLT criteria (mostly grade 3 reversible hepatic enzyme elevations) occurred with eganelisib 60 mg in later treatment cycles. In combination, the most common treatment-related grade ≥3 toxicities were increased AST (13%) and increased ALT and rash (10%). Treatment-related serious AEs occurred in 5% of monotherapy patients (grade 4 bilirubin and hepatic enzyme increases in one patient each) and 13% in combination (pyrexia, rash, cytokine release syndrome, and infusion-related reaction in ≥2 patients each). Antitumor activity was observed in combination, including patients who had progressed on PD-1/PD-L1 inhibitors.
Conclusions: On the basis of the observed safety profile, eganelisib doses of 30 and 40 mg once daily in combination with PD-1/PD-L1 inhibitors were chosen for phase 2 study.
This article was highlighted in the June 15 issue.
Journal: Molecular Cancer Research
Interdependence of SS18-SSX-driven YAP1 and β-catenin Activation in Synovial Sarcoma
Synovial sarcoma, a rare malignant soft tissue tumor, is characterized by a specific chromosomal translocation t(X;18). The resulting chimeric SS18-SSX fusion protein drives synovial sarcoma pathogenesis by integrating into the BAF complex and dysregulating gene transcription. Because previous functional analyses revealed a connection between SS18-SSX and the activity of the transcriptional coregulators YAP1/TAZ and β-catenin, respectively, this study examined a potential interdependence between these essential effector proteins in synovial sarcoma. In a large cohort of synovial sarcoma tissue specimens, IHC analyses revealed a substantial subset of synovial sarcoma with concurrent nuclear accumulation of YAP1/TAZ and β-catenin. In vitro, small-molecule inhibitor treatment, RNAi-mediated knockdown, and vector-based overexpression assays demonstrated that YAP1, TAZ, and β-catenin transcriptional activity is not only stimulated by the SS18-SSX fusion protein, but that they also mutually enhance each other’s activation. These analyses showed the highest cooperative effect with overexpression of YAP1 in combination with β-catenin. Coimmunoprecipitation experiments detected nuclear interactions between YAP1, β-catenin, and the SS18-SSX fusion protein, the latter being an integral part of the BAF complex. Disruption of BAF complex assembly affected the coregulation of YAP1 and β-catenin, indicating that this chromatin remodeling complex plays a crucial role for interdependent YAP1 and β-catenin activation in synovial sarcoma cells.
Implications: This study provides deeper insights into synovial sarcoma tumor biology demonstrating a mutual dependence between YAP1/TAZ and β-catenin transcriptional activity and a complex interplay with the SS18-SSX fusion protein within the BAF complex.
This article was highlighted in the June issue.
Journal: Molecular Cancer Therapeutics
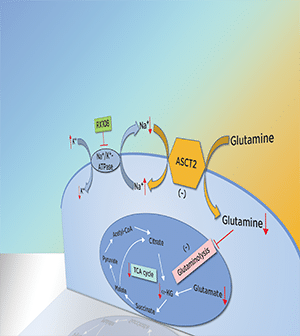
The poor prognosis and limited therapeutic options for human hepatocellular carcinoma (HCC), the most common form of liver cancer, highlight the urgent need to identify novel therapeutic modalities. Here, we describe the antitumor activity and underlying molecular mechanisms of a novel Na+/K+-ATPase inhibitor RX108 in human HCC cells and its xenograft model. RX108 dose-dependently inhibited HCC cell proliferation in vitro and tumor growth in a xenograft mouse model, and that the inhibition was associated with induction of apoptosis. Mechanistically, RX108 significantly downregulated alanine serine cysteine transporter 2 (ASCT2) protein expression and reduced glutamine and glutamate concentration in HCC cells and tumors. In addition, RX108 exposure led to a significant decrease in cell energy metabolism in Huh7 and Hep3B cells, including decreased levels of glutathione, NADH, NADPH, and mitochondrial respiration oxygen consumption rate. Furthermore, HCC cells exhibited evidence of glutamine addiction; the antiproliferative effect of RX108 was dependent on glutamine transport. Clinically, elevated ASCT2 mRNA expression in HCCs was associated with unfavorable survival. Taken together, these findings reveal a novel approach to target glutamine metabolism through inhibiting Na+/K+-ATPase and provide a rationale for using RX108 to treat HCC in patients whose tumors express ASCT2 at high levels. RX108 is currently under clinical development.
This article was highlighted and featured on the cover of the June issue.
Journal: Cancer Research Communications
Multiple Germline Events Contribute to Cancer Development in Patients with Li-Fraumeni Syndrome
Li-Fraumeni syndrome (LFS) is an autosomal dominant cancer-predisposition disorder. Approximately 70% of individuals who fit the clinical definition of LFS harbor a pathogenic germline variant in the TP53 tumor suppressor gene. However, the remaining 30% of patients lack a TP53 variant and even among variant TP53 carriers, approximately 20% remain cancer-free. Understanding the variable cancer penetrance and phenotypic variability in LFS is critical to developing rational approaches to accurate, early tumor detection and risk-reduction strategies. We leveraged family-based whole-genome sequencing and DNA methylation to evaluate the germline genomes of a large, multi-institutional cohort of patients with LFS (n = 396) with variant (n = 374) or wildtype TP53 (n = 22). We identified alternative cancer-associated genetic aberrations in 8/14 wildtype TP53 carriers who developed cancer. Among variant TP53 carriers, 19/49 who developed cancer harbored a pathogenic variant in another cancer gene. Modifier variants in the WNT signaling pathway were associated with decreased cancer incidence. Furthermore, we leveraged the noncoding genome and methylome to identify inherited epimutations in genes including ASXL1, ETV6, and LEF1 that confer increased cancer risk. Using these epimutations, we built a machine learning model that can predict cancer risk in patients with LFS with an area under the receiver operator characteristic curve (AUROC) of 0.725 (0.633–0.810).
Significance: Our study clarifies the genomic basis for the phenotypic variability in LFS and highlights the immense benefits of expanding genetic and epigenetic testing of patients with LFS beyond TP53. More broadly, it necessitates the dissociation of hereditary cancer syndromes as single gene disorders and emphasizes the importance of understanding these diseases in a holistic manner as opposed to through the lens of a single gene.
Source link
#Editors #Picks #June #Highlights #AACR #Journals



