Does a diagnosis of severe physical illness elevate suicide risk?

Being diagnosed with a severe physical health condition is a psychological blow. We know that it can lead to serious depression, but does it also increase the risk of suicide? Does that risk change over time? Those are the questions Nafilyan and colleagues (2023) set out to explore.
Four severe conditions were considered: low-survival cancers, chronic ischaemic heart disease, chronic obstructive pulmonary disease (COPD), and degenerative neurological conditions such as Huntington’s disease. More than 47 million people in England participated via census data that was linked to hospital and death registration records.

When a person is diagnosed with a severe physical health condition, are they at increased risk of suicide?
Methods
For this investigation, Nafilyan et al. created a novel dataset that linked the 2011 Census to National Health Service hospital and death registration records. The dataset included 47,354,696 people who had completed the 2011 Census and were still alive in England on 1 January 2017. Those in the linked dataset who were subsequently diagnosed with one of four severe physical health conditions were matched to individuals without such diagnoses.
Matching criteria were sociodemographic factors including age, sex, ethnicity, religion, index of multiple deprivation, and region of residence. To be eligible as a match, an individual had to be alive at the time of diagnosis of the severe illness, and could not have been diagnosed with a severe illness themself. The matching was implemented in Python 3. The extraordinary size of the database allowed researchers to create matches with an overall linkage rate of 91%.
The researchers used the Aalen–Johansen estimator to calculate the incidence of suicide in patients and matched controls. Using inverse probability weighting, they adjusted for other potential factors that were not included in matching by fitting a logistic regression model for previous mental health problems, educational standing (degree/no degree), health in 2011 (disability or poor health), and marital status.
The period under study began at the first hospitalisation for one of the four terminal conditions. Follow-up ended on the earliest date of death (whether by suicide or another cause) and end of study (31 December 2021). Matched controls were assigned the diagnosis date of the patient with whom they were matched. All individuals who did not die were followed for at least 640 days. The survival analysis was conducted using R 3.6.
Results
In this cohort study of over 47 million people, those who were diagnosed with a life-threatening condition were two to three times more likely than matched controls to die by suicide. The increase in risk was most pronounced in the first six months after diagnosis or first treatment.
It is important to stress that these numbers (two to three times more likely) are relative risk statistics, which can often be misleading. For clarity, we have presented the absolute risk numbers below for each condition. If you want to find out more about the difference between relative and absolute risk, check out this short video featuring David Spiegelhalter.
Low-survival cancers
- Six months after diagnosis, the suicide rate for low-survival cancer patients was 16.6 per 100,000 (N=30), compared to 5.7 per 100,000 matched controls.
- One year after diagnosis, the cumulative suicide rate was 21.6 per 100,000, compared to 9.5 per 100,000 for the matched controls.
- The risk for suicide in low-survival cancer patients was highest in the first few months following diagnosis but remained elevated for the following two years, while the suicide risk for matched controls was constant.
COPD
- Six months after diagnosis of COPD, the suicide rate was 13.7 per 100,000 (N=128), compared to 5.6 for matched controls.
- One year after diagnosis, the cumulative suicide rate was 22.4 per 100,000, compared to 10.6 per 100,000 for matched controls.
- The risk for suicide in COPD patients was highest in the first few months following diagnosis but remained elevated for the following two years, while the suicide risk for matched controls was constant.
Chronic ischaemic heart disease
- Six months after diagnosis of chronic ischaemic heart disease, the suicide rate was 11.0 per 100,000 (N=156), compared to 4.2 for matched controls.
- One year after diagnosis, the cumulative suicide rate was 16.1 per 100,000, compared to 8.8 per 100,000 for matched controls.
- The risk for suicide in patients with chronic ischemic heart disease was highest in the first few months following diagnosis but was similar to that of matched controls in the second year after diagnosis.
Degenerative neurological conditions
- Patients diagnosed with a degenerative neurological condition were at particularly high risk of suicide, with a one-year suicide rate of 114.5 per 100,000 (N=11), with no suicides reported in the matched controls.
- The researchers stated that this estimate was imprecise due to the low numbers. There are far fewer subjects in this group (10,320 diagnosed with a degenerative neurological condition, as compared with 1,383,016 with chronic ischemia, 885,716 with COPD, and 176,709 with low-survival cancer).
Risk patterns were similar in both men and women.
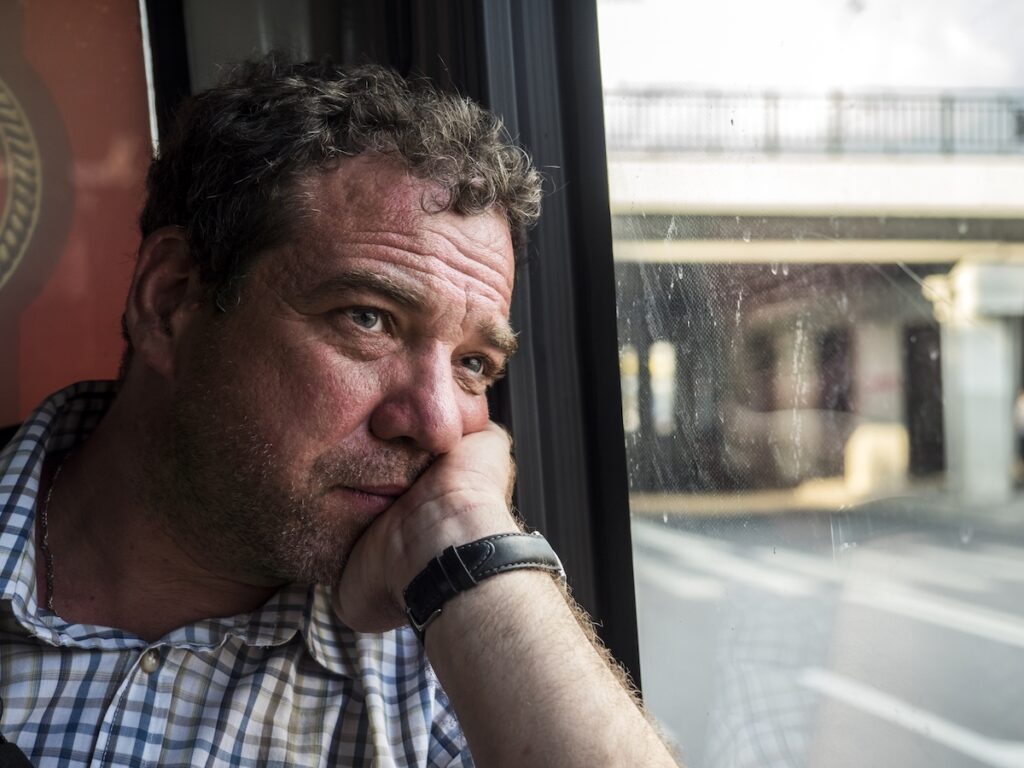
Being diagnosed with a severe physical illness can have fatal psychological consequences for some people.
Conclusions
The authors conclude:
Further research is needed to understand the mechanisms driving the elevated risk of suicide and help provide the best support to these patients. In the meantime, providing better support to recently diagnosed patients is critical to help people cope with a severe condition diagnosis.
Implications of these findings include the importance of attending to the psychological needs of patients when diagnosing them with a severe life-threatening disease, for at least the two years following the diagnosis. The physical health needs of these patients are obviously important, but their psychological needs should not be ignored.

Clinicians need to consider the elevated suicide risk of patients recently diagnosed with severe physical health conditions and ensure psychological support.
Strengths and limitations
It’s extremely valuable to understand the psychological impact on a patient when they’re diagnosed with a severe physical health condition. The authors have added to this understanding by showing the substantially elevated risk of suicide when someone is diagnosed with a low-survival cancer, chronic ischemic heart disease, chronic obstructive pulmonary disease, or a degenerative neurological condition.
The method they devised allowed them to be conclusive in their findings. By linking census data to mortality data, it gave them access to extensive records for over 47 million people. They were therefore able to identify exceptionally large numbers of people diagnosed with each condition, and also able to provide close matches for each identified patient.
However, suicide is not always reliably reported. It may be recorded in official records as a natural outcome of a fatal illness, an accidental overdose of medications, or be masked in some other way. Matched controls are of course subject to the same concern with the under-reporting of suicide, but (given the findings of this study) this will almost certainly be less frequent. The findings may therefore be a low estimate of the actual impact of the diagnoses under examination.
The authors don’t address the deeper philosophical, ethical, and legal questions implicit in a study like this, such as whether suicide might be a reasonable choice following a terminal diagnosis, especially where the dying process is predicted to be painful and debilitating. Further, might the findings suggest an important role for legalised assisted suicide?
The authors might have pointed out that data had been generated but not analysed on many topics, including religion. Why, for example, are Christians so much more likely to be diagnosed with each of the four severe conditions than people from all other religious affiliations and those who describe themselves as having no religion? Similarly, the dataset demonstrates large ethnic, socioeconomic, and regional differences in the diagnostic rates of the four severe conditions under study. This raises many questions that the authors might have pointed out as valuable for future study. For example, why are White British and Irish people so much more likely than others (Asian, Black, Chinese, mixed race, etc.) to be diagnosed with the four severe conditions? Are White British and Irish so much more susceptible to each of these conditions? Or are the conditions frequently missed or under-diagnosed in Asian, Black, Chinese, and mixed race populations? The data raises many questions, each of which is worth exploring further.

The findings generated here also raised ethical questions concerning demographic differences in diagnostic rates and access to assisted suicide.
Implications for practice
As Nafilyan et al. point out, the findings of this study emphasise the necessity of mental health professionals’ involvement in collaborative teams, working with medical health professionals to support patients in coping with severe physical health diagnoses.
When medical training and practice occur in increasingly fragmented and narrower specialties and subspecialties, it’s easy for practitioners to lose sight of the whole patient and focus on the disease in which they have expertise. There is certainly an essential role for narrowly specific medical expertise, but these findings suggest that that would be best put into a holistic context, such that patients are given both the medical and the psychological support they need.
The recommendations emerging from this study underline the importance of the study conducted by S Moon et al. (2022) that considered the complex supports necessary following diagnosis of a serious physical health condition. They showed that individuals vary tremendously in their interpretation of their condition, the supports available, and many other factors that affect their ability to thrive. Medical and psychological practitioners working with patients diagnosed with a severe condition such as those studied by the authors would benefit from familiarising themselves with the recommendations in the Moon et al. study.

Compassionate public policy needs to promote collaborative care teams to support patients’ optimal overall health.
Statement of interests
No conflicts.
Links
Primary paper
Nafilyan, V., Morgan, J., Mais, D., Sleeman, K. E., Butt, A., Ward, I., Tucker, J., Appleby, L., & Glickman, M. (2023). Risk of suicide after diagnosis of severe physical health conditions: A retrospective cohort study of 47 million people. The Lancet Regional Health – Europe, 25, 100562. https://doi.org/10.1016/j.lanepe.2022.100562
Other references
Carroll S, Moon Z, Hudson J, Hulme K, & Moss-Morris R (2022) An evidence-based theory of psychological adjustment to long-term physical health conditions: applications in clinical practice. Psychosomatic Medicine 2022 10.1097/PSY.0000000000001076
Matthews D (2022) A long-term physical health condition changes everything: therapeutic responses to psychological distress must change too #BABCP2022
Source link
#diagnosis #severe #physical #illness #elevate #suicide #risk

