Cancer Research UK – Science blog
When a tumour grows, it can’t grow in isolation.
Instead, it’s surrounded by what’s called the tumour microenvironment, a network of cells, molecules and blood vessels that provide the tumour with structural support and the nutrients it needs to keep growing.
You can think of the tumour microenvironment as a scaffold that the tumour uses to support itself.
Part of that microenvironment is the extracellular matrix (ECM), which comprises of things you might have heard of like collagen, that it uses to defend itself from immune attacks among other things.
Another thing that you can find in the ECM might also sound familiar: hyaluronic acid.
You might have heard of hyaluronic acid (HA) in the context of skincare. That’s because hyaluronic acid absorbs water. In your skin, that can be a good thing. HA keeps your skin plump by retaining water. But in a tumour, that’s not such a positive.
By binding to water molecules, HA causes swelling within the tumour, which in turn can make tumour blood vessels collapse, cutting off its supply of blood and oxygen. That’s no problem for the tumour; tumours can survive in low oxygen conditions, known as hypoxia. But it is a problem for treatment.
Restricting the blood supply also makes getting drugs into tumours more difficult. That, in turn, makes chemotherapies less effective in these tumours as the drugs can’t reach their target.
In breast tumours, often the ones with a denser ECM have poorer prognosis, including a higher chance of spreading to another part of the body, known as metastasis.
That makes hyaluronic acid a prime target for new therapeutics. If we can degrade it in situ, we can dissolve some of this dense ECM and improve drug delivery to these tumours.
Reading the response
We do have some candidates for a drug that targets hyaluronic acid, including one called PEGPH20 that degrades hyaluronic acid and helps to decompress the blood vessels within the tumour.
The problem we’ve encountered so far with testing this drug is that it’s been administered in combination with chemotherapy in a clinical trial setting, and the method used to tell whether it was working, taking a biopsy of the tumour, was done after both drugs were given.
That makes things complicated, as if a tumour didn’t respond to treatment, it was unclear whether that was because PEGPH20 hadn’t worked, or whether the tumour was resistant to the chemotherapy.
What we need is a marker we can measure to quickly determine whether drugs like PEGPH20 are working in degrading hyaluronic acid first, before we administer any additional treatment.
That way, patients who aren’t responding to PEGPH20 can be spared unnecessary chemotherapy, and alternative drugs can be trialled in patients who do respond to PEGPH20 but don’t respond to the treatment they’re given.
And now, researchers at the Institute of Cancer Research (ICR) have recently published results of a study showing us one we can use.
Finding the right marker
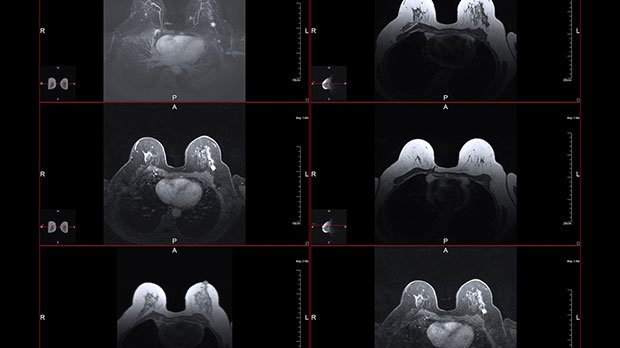
“Our research is about finding imaging biomarkers that will tell you whether a patient has responded or not responded to treatment,” says Dr Emma Reeves, who performed the studies during her Cancer Research UK funded PhD studentship. “And to do that, we used MRI.”
Specifically, the team used what’s called multiparametric MRI. That means that on top of the usual anatomical images an MRI scanner takes, it can take additional measurements of tissue function to give us greater insight into the tumour being visualised.
In this case, the team used elastography, a technique that measures tissue stiffness, and diffusion-weighted imaging, that can show us how water molecules are able to move within a tissue.
Measuring the stiffness of tissue might sound odd, but malignant breast tumours are often associated with a dense ECM high in collagen, which makes the tissue stiffer. If the tumour is responding to treatment, the tissue then typically softens.
Similarly, being able to see whether water is retained in these tissues can show us whether HA is still present. The acid binds to the water, but if it’s been successfully degraded by PEGPH20, the ECM loses water and constricts, which can be seen using diffusion-weighted imaging.
“An MRI is completely non-invasive, and you can look at multiple time points throughout the treatment. With a biopsy, you just get a small sample of the tumour, whereas with the MRI you can look at the whole tumour and see the response to treatment,” explains Professor Simon Robinson, Team Leader for Pre-Clinical MRI at the ICR.
“Or if there are metastases, you can see the response of different tumours.”
So, they added these extra tests to a standard MRI scan with the aim of identifying an imaging biomarker that can tell us whether drugs like PEGPH20 are working.
And they found one.
ADC
It’s called the apparent diffusion coefficient, or ADC for short. It’s one of the additional biomarkers that multiparametric MRI can measure.
ADC is sensitive to the amount and movement of water in the tissue being examined and can give us information on tissue properties like equilibrium of water inside vs outside a cell. In tumour tissues, the movement of water is restricted by the dense ECM.
Breast tumours with different levels of HA were treated with PEGPH20, and the researchers then imaged the response to this treatment with MRI.
What they observed was that ADC had decreased in tumours treated with PEGPH20 vs those treated with just saline water, which indicates that water had been lost from the tumour, i.e., the tumour was responding to the treatment.
What’s more is that even in tumours that had less accumulation of HA the decrease in ADC was observed, showing that ADC is a sensitive biomarker that can also be used to detect smaller changes in water content.
Therefore, ADC shows strong potential to be a biomarker for the monitoring of stromal targeted therapies. And the additional benefit of this technique is that recording ADC only adds few minutes to a routine patient MRI scan.
“ADC is a measurement that’s routinely used in the clinic,” says Reeves. “If PEGPH20 was to go back into a clinical trial, I think it could be relatively easily included in that imaging regime.”
Speeding up drug development
Drugs similar to PEGPH20 are still in the development phase. They’ll need to be rigorously tested in further clinical trials before they can reach patients in the clinic. But targeting the tumour microenvironment and ECM is a rapidly growing area of interest in cancer research, and it isn’t specific to breast cancer.
“The premise of HA absorbing water, then getting degraded and releasing that water away from the tumour would be the same for other solid tumour types that typically exhibit a dense ECM, such as pancreatic cancer,” says Reeves.
“Perhaps there would be a bit of a difference with something like a brain tumour where the microenvironment is completely different. But that doesn’t mean it wouldn’t work, it just means that maybe the ADC values would be quite different that we’re getting out of the MRI.”
If we can implement new techniques like this, that add quick, simple and non-invasive steps to already routinely used tests in the clinic, we can accelerate the development of stromal targeted therapies and improve the effectiveness of chemotherapies in these dense tumours.
Jacob
Source link
#Cancer #Research #Science #blog



