Cancer Research UK – Science blog
Getty Images
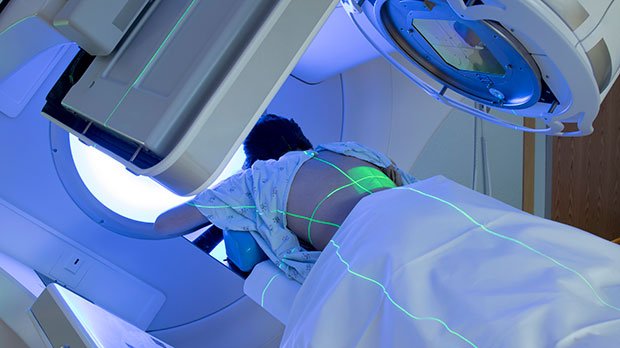
Radiotherapy is a key treatment for many people affected by cancer, and it plays an important role in both curing early-stage cancer and in helping to ease some symptoms for people with terminal illness. But, like many other cancer services in the UK, radiotherapy is facing huge challenges.
So, over the autumn, Cancer Research UK’s Policy Development team surveyed people who have either received radiotherapy or supported someone going through it in England to understand how people experience radiotherapy treatment.
We were grateful and impressed to receive over 100 responses. And we learned a lot!
We learned that, while people generally have good experiences of radiotherapy, many still feel they waited too long before starting their treatment. And the majority of respondents said that starting treatment quickly after diagnosis is the most important aspect of radiotherapy.
The survey responses, along with insights from radiotherapy experts and staff, will now play an important role in how we persuade the UK Government and NHS England to improve radiotherapy services. Today we’re publishing a new policy position statement to share what we’ve found out, and the improvements we need to see.
Positive treatment experiences
Through our survey, we were happy to learn that people who’ve had radiotherapy in England are generally satisfied with their treatment experience. Over 80% of respondents said they had received the right high-quality radiotherapy treatment for their cancer.
Over 2 in 3 people agreed they got all the support and information they needed from clinicians during their radiotherapy treatment. Around 1 in 6 disagreed.
On the other hand, some felt they were not given adequate information about what to expect after treatment, especially in terms of immediate and late side effects. Asked what would have made their experience of radiotherapy better, one respondent said: “More info about what to expect afterwards. I think my expectations were unrealistic and this has made the post treatment period extremely difficult for me.”
People are waiting too long for diagnosis and treatment
While the survey generally showed positive treatment experiences, we know radiotherapy services face huge challenges that need to be addressed.
Cancer waits for diagnosis and treatment are getting longer and NHS England’s waiting time targets are missed month after month. In February, only 92% of patients started cancer treatment within 31 days of diagnosis, again missing the NHS England target of 96%. This target has not been met since December 2020.
This is worrying because timely treatment can affect outcomes. And we know from our survey that a quick start to treatment is the aspect of radiotherapy that people find most important.
There is no doubt that pressures from the COVID-19 pandemic are contributing to longer waits. Our survey also showed that most of the people who felt they waited too long to start their treatment had radiotherapy in the last 36 months – during the pandemic period.
But COVID-19 is only part of the reason. The main driver of long waits is a severe lack of staff.
The shortfall in the radiotherapy workforce is a longstanding issue that got worse during COVID-19. And demand for radiotherapy is only set to grow in the future.
This is because be diagnosed with cancer and need radiotherapy treatment. As some early-stage cancers can be cured with radiotherapy, the ongoing push for earlier diagnosis could also increase demand.
Lack of radiotherapy staff
Three of the key professions involved in radiotherapy – clinical oncologists, therapeutic radiographers, and medical physicists – are short on staff. Clinical oncologists had a staff shortfall of 17% in 2021, which according to the Royal College of Radiologists is expected to grow to 26% by 2026. Both therapeutic radiographers and medical physicists had a staff shortfall of around 8%.
This chimes with what we’ve heard from radiotherapy experts and staff: almost everyone mentioned workforce issues as the most important challenge for radiotherapy services.
The radiotherapy workforce, like the wider NHS workforce, showed incredible resilience and endurance during the COVID-19 pandemic, keeping most radiotherapy services running during a time of severe pressure and stress. But the pressure from the pandemic, and the backlog it has created, means staff burnout is now a serious issue.
In 2021, 100% of radiotherapy service heads said they are concerned about workforce morale, stress and burnout. And that threatens staff retention for an already stretched workforce.
That’s why we continue to tell the Government that their upcoming long-term workforce plan must be transparent, fully funded, and include reforms to improve staff retention in the NHS and particularly within cancer services.
Innovation delivers kinder and more effective treatment
We also learned that people with cancer find access to innovative types of radiotherapy very important.
We asked people to rank the most important aspects of radiotherapy treatment. Access to innovative radiotherapy was ranked the second highest, with almost half of respondents including it in their top three.
And despite workforce shortages, ground-breaking research into new radiotherapy technologies and techniques – such as proton beam therapy, hypofractionation, stereotactic ablative radiotherapy, and molecular radiotherapy – has led to both kinder and more effective treatment for people with cancer in the NHS in England.
There is no doubt that radiotherapy is seeing lots of breakthroughs that are right at the cutting-edge of medical innovation. But delivering innovative radiotherapy is not cheap or simple.
Although new techniques often require modern equipment, the NHS doesn’t automatically replace older radiotherapy machines when they reach the end of their lifespan. That means some machines are still in use when they should have been replaced. Many of the experts we spoke to told us they prefer a system of automatic machine replacement, so we’re calling for the Government to implement this.
Delivering new techniques also requires staff training, new IT infrastructure, and quality assurance – and, of course, staff time and capacity.
This is a fundamental challenge – and one we think can only be addressed if researchers, research funders, NHS staff, NHS decision-makers, and patients have a shared vision of the most important innovations of the future.
A long-term plan for radiotherapy
That’s why today we’re publishing a new policy position statement that calls for the Government and NHS England to make specific, targeted improvements to radiotherapy services, so people with cancer have timely access to advanced and innovative radiotherapy now and in the years to come.
Most importantly, we’re calling on the Government and NHS England to work on a new longer term strategic direction for radiotherapy services in England. That needs to be formed from conversations and collaborations between NHS staff, researchers, charities, industry, NHS decision-makers, and ministers.
Click through to read the policy position statement in full.
But our work doesn’t stop there.
Our Manifesto for Cancer Research and Care
As we approach a General Election, expected next year, UK political parties are turning their minds to longer term policy, as they prepare to convince the electorate that they have the answers to the country’s biggest challenges.
This is an important opportunity to remind political parties of the importance of long-term strategic planning for cancer treatment, and indeed right across cancer services.
That’s why Cancer Research UK’s Policy Department are developing a Manifesto for Cancer Research and Care – a transformational, long-term view of how to improve cancer research and care in the UK.
Source link
#Cancer #Research #Science #blog



