One CAR T-Cell Therapy for Blood Cancers?
,
by Carmen Phillips
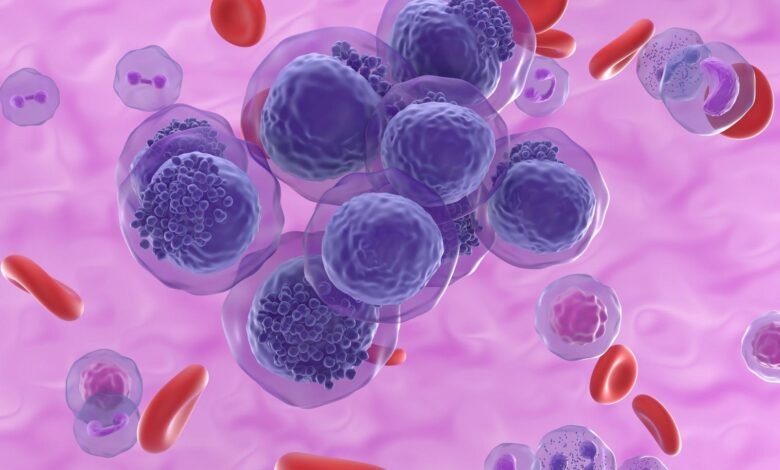
In the Lord of the Rings, there was “one ring to rule them all.” Now, a team of researchers is developing their own single ruler, an approach to CAR T-cell therapy that could treat all forms and types of blood cancer.
In experiments in mouse models of different blood cancers, the treatment rapidly eliminated tumors, including in mice with acute myeloid leukemia (AML), a difficult-to-treat type of blood cancer for which researchers have struggled to develop effective immunotherapies.
There was also no evidence of serious side effects in the animals. And, finally—and distinctly from the standard approach to current CAR T-cell therapies—it provided the mice with a healthy supply of new blood cells.
Results from the study were published August 31 in Science Translational Medicine.
Developed by a research team at the University of Pennsylvania Perelman School of Medicine, the treatment relies on a newer form of the gene-editing technology CRISPR, called base editing.
But in a unique twist for CAR T-cell therapy, it’s not only T cells that undergo genetic engineering. The treatment also involves engineering healthy hematopoietic stem cells. These are the “immature” cells that generate all the body’s blood cells, including immune cells (like T cells), and form the basis for the stem cell transplants already commonly used to treat many blood cancers.
In the new treatment approach, the CRISPR editing results in a slight change to a protein, called CD45, that sits on the surface of both the CAR T cells and the stem cells.
This impostor CD45 protein, in turn, produces a maneuver straight out of another fantasy novel: It provides noncancerous cells with a cloak of invisibility. The proposed result of all of this work: A CAR T-cell therapy that can kill any type of blood cancer cell, and only blood cancer cells, while giving patients a healthy blood and immune system.
The approach, the researchers believe, could expedite progress with CAR T-cell therapy by eliminating the need to go through the laborious and time-consuming process of developing and testing single therapies for specific blood cancers, which is the case with the currently approved CAR T-cell treatments.
Sarah Tasian, M.D., chief of the Hematological Malignancies Program at Children’s Hospital of Philadelphia, who was not involved in the study, called the treatment approach “intriguing.” Dr. Tasian cautioned, however, that she’d like to see further testing in other animal models, including careful analysis of the treatment’s safety.
According to one of the study’s lead investigators, Saar Gill, M.D., Ph.D., the team is already engaged in additional testing and other steps needed to advance this treatment approach.
“We’re very determined to get this into a clinical trial,” Dr. Gill said. “It’s the only way we’ll know if it’s going to work.”
A different approach to finding a target antigen
From their inception, creating CAR T-cell therapies has been a complicated process.
It involves genetically manipulating T cells collected from patients so that the cells produce specialized receptors on their surface, called CARs. Once the engineered T cells are infused back into patients, their CARs latch on to cancer cells via a specific protein on their surface, known as an antigen, and kill them.
But a limitation of these treatments is that their target antigen must only be found on cancer cells and not, or in very limited amounts, on other healthy cells. If the antigen is commonly found on other cells, significant collateral damage—in the form of potentially serious side effects—can occur.
Typically, these target antigens are “lineage antigens,” which are specific to the type of cell on which they’re produced.
In acute lymphoblastic leukemia (ALL), for example, the approved CAR T-cell therapies are engineered to latch onto a lineage antigen found on nearly all B cells called CD19. For multiple myeloma, the approved CAR T-cell therapy targets a lineage antigen on plasma cells called BCMA.
These CAR T-cell therapies can be highly effective, even curing some people with very advanced disease for whom all other therapies no longer work.
“We hit home runs with CD19 and BCMA,” said Saad Kenderian, M.D., of the Mayo Clinic Comprehensive Cancer Center in Minnesota, who was not involved in the study. But finding similar target antigens for the many other types of blood cancer has proved extremely difficult, Dr. Kenderian explained.
Because CD45 is a lineage antigen for most types of blood cells, including white blood cells, it would seem to be a poor candidate against which to develop a CAR T-cell therapy.
But its near universal presence also makes CD45 uniquely attractive, Dr. Gill said.
If the team’s goal was to create a single CAR T-cell therapy that could treat virtually all cancers that form in blood cells, as far as a target antigen was concerned, he said, “that was the one.”
Editing in destruction and protection
Developing this new approach to CAR T-cell therapy required adding new layers of complexity to this already complex process.
Dr. Gill and his colleagues from Penn’s Abramson Cancer Center first identified the specific sites on the CD45 protein where different CARs they had developed could bind. These spots are called epitopes.
The next step was finding one such epitope that could be altered while still allowing CD45 to
function normally in blood cells. The ideal alteration would also change the protein just enough so that it wouldn’t be recognized by a CD45-targeting CAR.
Further experiments identified what the team judged to be the ideal epitope to move forward with. And that’s where the CRISPR base editing came in to play. They used the technology to make a tiny alteration in the gene responsible for producing CD45, so that the protein had the necessary changes at this precise epitope—which they called “epitope editing.”
The stage was then set for a double dose of engineering. First, creating T cells that produce both the CD45-binding CAR and the altered version of CD45, allowing the T cells to target cells with normal CD45 while simultaneously protecting themselves from such an attack.
The hematopoietic stem cells, meanwhile, only underwent epitope editing. As a result, the blood cells they generated after being delivered into the body would only produce the impostor CD45 on their surface, also protecting them from the CAR T cells.
Killing cancer cells, but not other CAR T cells or blood cells
In lab experiments, the epitope-edited CD45-targeted CAR T cells worked as intended, killing several different types of blood cancer cells, but not killing each other (called “fratricide”).
In mice, the treatment shrank tumors and, as in the lab experiments, the T cells did not turn on each other.
Some of the engineered T cells also stuck around in the mice. When more AML cells were introduced into the animals months later, the CD45-targeted CAR T cells quickly jumped into action and eliminated them.
Altering CD45 in the hematopoietic stem cells also worked as planned. In lab experiments and in mice, they formed healthy white blood cells. And when given to mice prior to treatment with the epitope-edited CAR T cells, the resulting blood cells were shielded from attack.
And Dr. Gill highlighted another important finding: The blood cells with the epitope-edited CD45 seemed to be functioning normally.
Heading for clinical trials
The Penn team is not alone in using epitope-editing as a means of expanding the reach of CAR T-cell therapies. Researchers at Dana-Farber Cancer Institute and Harvard Medical School published a somewhat similar study in Nature on August 30, although it was focused exclusively on AML.
In that study, the researchers successfully used epitope editing on hematopoietic stem cells to cloak them from CAR T cells engineered to target a few different antigens commonly found on AML cells.
Further testing in models of high-risk blood cancers, including lymphomas with features that make them less likely to respond to standard treatments, would be good to see, Dr. Tasian said. Innovative approaches for treating these high-risk blood cancers “remain critically important to address,” she said.
Meanwhile, the Penn research team, led by Carl June, M.D., a CAR T-cell therapy pioneer, is already working on advancing their universal treatment approach to clinical trials.
“We think it’s doable within 2 years,” Dr. Gill said.
Details of how it will be run are yet to be figured out, he continued. For example, whether the T cells and stem cells to be edited will be collected from patients themselves (which is the case with the currently approved CAR T-cell therapies) or, instead, if they will come from healthy donors.
These and other issues need to be worked out, said Dr. Kenderian. But he believes that, based on results from the two recent studies and some related studies, it should be full steam ahead for this approach.
“The safety, the precision of editing, and the efficacy of the CAR T cells is quite compelling,” he added. “And, in my mind, enough so to move [this approach] into a human trial.”
Source link
#CAR #TCell #Therapy #Blood #Cancers



