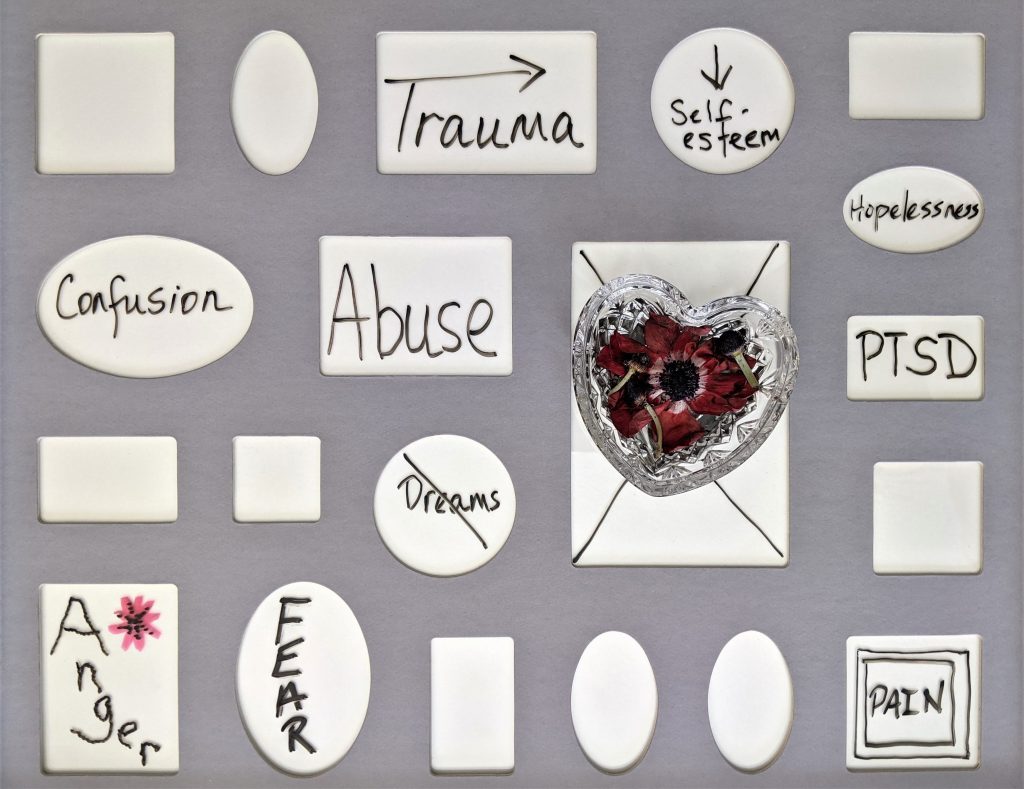
Trauma transdiagnostic risk mental health

Perhaps unsurprisingly, trauma and post-traumatic stress disorder (PTSD) go hand-in-hand. Prior trauma exposure is required to receive a diagnosis of PTSD. However, trauma exposure, particularly during childhood, has also been associated with a range of other mental health disorders throughout the lifespan (Green et al. 2010; Kessler et al., 2010; McLaughlin et al., 2012). In light of estimations suggesting that 70% of the adult population can expect to experience at least one traumatic event during their lifetime (Benjet et al., 2015), prevention, intervention, and treatment strategies for addressing mental health problems in the aftermath of trauma exposure are essential.
Mental health services worldwide operate using discrete categories: if an individual presents with symptoms X, Y, and Z, this symptom profile corresponds to diagnosis A, and they should be treated using treatment B. However, research has shown significant overlap and connections among 50% of the symptoms of mental health disorders (Borsboom et al., 2011). If symptoms are shared across disorders, treatments that target these shared symptoms could plausibly be used in the treatment of a range of mental health disorders; this is the core aim of transdiagnostic approaches to treatment.
Trauma exposure has been associated with long-lasting negative impacts on an individual’s wellbeing and functional abilities, including increased engagement in health risk behaviours, and most individuals do not or are unable to access treatment (Huang et al., 2014). This blog will summarise a recent meta-analysis conducted by Hogg et al. (2022) that aimed to examine trauma as a transdiagnostic risk factor across mental health disorders and explore the potential utility of a trauma-focused transdiagnostic treatment.

Mental health services worldwide operate using discrete categories, but significant symptom overlap between different mental health disorders suggests that transdiagnostic approaches may be plausible.
Methods
Hogg and colleagues (2022) searched three electronic databases to identify systematic reviews and meta-analyses written in English or Spanish that evaluated the association between psychological trauma and at least one diagnosed mental health disorder. Papers were required to include a control group, meaning participants fell into one of four groups:
- Disorder and trauma
- Disorder and no trauma
- No disorder and trauma
- No disorder and no trauma.
Articles were independently screened by two researchers by title and abstract, and then by full text. Study quality judgements and data extraction were carried out by two independent researchers and discrepancies were discussed at a consensus meeting. Reference lists of papers that reached full-text review were also manually searched for additional papers.
The authors conducted a random-effects meta-analysis of the relative risk (RR) or odds ratio (OR) of developing a mental health disorder in those exposed to psychological trauma compared to those not exposed to psychological trauma. Each included paper was classified in terms of the credibility of each association (convincing, highly suggestive, suggestive, or weak) and TRANSD criteria (Fusar-Poli, 2019) was used to assess whether psychological trauma can be defined as transdiagnostic.
Study characteristics
850 systematic reviews and meta-analyses were initially identified. Following screening, 14 papers met the inclusion criteria, encompassing 106 individual studies and 93,863 participants (16,277 cases and 77,586 controls). The included papers covered:
- Ten categories of psychological trauma: sexual abuse, physical abuse, emotional abuse, person under train incidents, military deployment to a war zone, disaster, illness diagnosis, parental loss during childhood, general traumatic event, and non-specific childhood trauma.
- A broad range of mental health disorders, grouped as follows by the authors: anxiety disorders (generalised anxiety disorder, panic disorder, and social anxiety disorder), psychosis (schizophrenia, schizoaffective disorder, psychotic disorder), bipolar disorder, PTSD, obsessive compulsive disorder (OCD), borderline personality disorder (BPD), major depressive disorder (MDD), and ‘other mental disorder’ (encompassing disorders where there were too few studies to investigate individually), as well as studies investigating any mental disorder.
Quality assessment
The authors used AMSTAR (Shea et al., 2007) to assess study quality:
- 3 of the included systematic reviews and meta-analyses were rated as poor quality using the AMSTAR tool
- 9 were rated as moderate quality
- 2 were rated as high quality.
Results
Overall, there was highly suggestive evidence of an association between any type of psychological trauma and any type of mental health disorder. There was almost triple the risk of diagnosis of any type of mental health disorder when exposed to any type of psychological trauma (OR=2.92; 95% CI=2.60 to 3.28).
Additionally, the authors conducted sensitivity analyses to separately explore this association for childhood trauma, which was referred to in 90 of the 106 included studies, and trauma during adulthood, which was referred to in only 12 of the 106 included studies (assessing only PTSD and MDD). There was highly suggestive evidence of an association between childhood trauma and any mental health disorder (OR=2.90; 95% CI= 2.58 to 3.26). In contrast, there was weak evidence of an association between exposure to trauma during adulthood and PTSD and/or MDD (OR=3.76; 05% CI=2.45 to 5.77).
The authors also conducted separate analyses for the associations between each of the trauma types and any psychiatric disorder, and each of the disorder types and any trauma exposure (see Table 1 for a summary of findings).
Table 1. Summary of findings
|
SPECIFIC TRAUMA & ANY DISORDER |
ANY TRAUMA & SPECIFIC DISORDER |
SPECIFIC TRAUMA & SPECIFIC DISORDER |
| Convincing evidence: physical abuse.
Highly suggestive evidence: sexual abuse, non-specific childhood trauma, and emotional abuse. Weak evidence: military deployment to a warzone, person under train, and disaster. |
Highly suggestive evidence: bipolar disorder, anxiety disorder, and psychosis.
Suggestive evidence: PTSD and ‘other’ category. Weak evidence: BPD, OCD, and MDD. |
Convincing evidence: exposure to emotional abuse and anxiety disorder, and exposure to physical abuse and anxiety disorder.
Suggestive evidence: exposure to sexual abuse and anxiety disorder, and exposure to non-specific childhood trauma and psychosis. 17 further associations met criteria for weak evidence. |
Finally, application of the TRANSD criteria demonstrated that psychological trauma is a transdiagnostic risk factor for mental health disorder across seven diagnostic categories.

The review found highly suggestive evidence of an association between any type of psychological trauma and any type of mental health disorder, with almost triple the risk of diagnosis when exposed to trauma.
Conclusions
This meta-analysis shows that exposure to any type of trauma was associated with triple the risk of being diagnosed with any mental health disorder. Additionally, this meta-analysis provides strong evidence that psychological trauma is a transdiagnostic risk factor across seven diagnostic spectra of mental health disorders, including anxiety disorders, bipolar disorders, depressive disorders, obsessive-compulsive disorders, personality disorders, schizophrenia spectrum disorders, and trauma- and stressor-related disorders.
The authors conclude that:
Our findings highlight the importance of psychological trauma as a public health concern, with implications for increased investment in prevention services and trauma-informed care across early intervention and treatment services, and open up the possibility for innovative treatment approaches based on psychological trauma as a transdiagnostic construct.
Findings from this umbrella review suggest that psychological trauma is a transdiagnostic risk factor for a range of mental health disorders.
Strengths and limitations
The authors aimed to explore whether psychological trauma is a transdiagnostic risk factor for mental health disorders, a topic of growing importance in terms of the prevention and intervention of mental health problems. This meta-analysis was conducted using rigorous procedures that are clear and replicable. Appropriate and reliable pre-existing criteria and guidelines were used during screening (PRISMA and MOOSE guidelines), assessing study quality (AMSTAR), assessing the credibility of the evidence (Ioannidis evidence criteria; Ioannidis, 2009), and assessing psychological trauma as a transdiagnostic risk factor (TRANSD). Additionally, the study protocol was pre-registered on PROSPERO prior to searching any databases.
However, there are some limitations that must be considered:
- Trauma exposure was, for the most part, assessed retrospectively using self-reports; trauma assessments could therefore have been affected by forgetting, misremembering, stigma, and subjective interpretations. The authors do acknowledge a study that found psychopathology during adulthood to be associated with subjective report of children’s maltreatment history rather than objective measures (e.g., court-documented evidence) and this limitation is more of a criticism of the current evidence-base as a whole, rather than this study specifically.
- As noted by the authors, three of the 14 included studies were rated as low quality according to the AMSTAR tool, indicating that a maximum of only four of AMSTAR’s eleven items related to robust, replicable, and unbiased methods were met.
- Although two researchers conducted screening, assessments of study quality, and extraction, they do not report inter-rater reliability at any of these stages.
- Sensitivity analyses were conducted to assess the associations between childhood trauma or trauma during adulthood and psychiatric disorders. However, the reasoning for combining these two types of traumas in the first place is unclear, particularly as none of the trauma types overlap both the childhood and adult trauma categories. Given there were more included studies exploring childhood trauma, this meta-analysis could have restricted their focus, enabling a more directed discussion of the prevention, intervention, and treatment of psychiatric disorders following childhood trauma.
- Finally, the authors created an ‘other disorder’ category which included disorders that had too few studies to explore individually. This category included attention-deficit and hyperactivity disorder (ADHD), conduct disorder, bulimia nervosa, and personality disorder, and any mood disorder. While this only affected one of the included systematic reviews, it assumes that trauma exposure influences the development of these disorders in the same way. These disorders should have been noted, but not included in analyses.
Trauma research often relies on retrospective self-reports which can be affected by forgetting and misremembering.
Implications for practice
Our frontline mental health services currently operate within the discrete categories outlined in the DSM-5 and the ICD-11, and despite growing research support for a transdiagnostic approach to the classification and treatment of mental health disorders, this does not look set to change any time soon. The categorical approach does have significant strengths for both practitioners and those diagnosed with mental health disorders, enabling clear links to be drawn between diagnoses and treatments (such as those outlined in the NICE guidelines) and between individuals who share the same diagnosis. However, in terms of the practicality of treatment, the categorical approach is lacking.
The demand for mental health treatments far exceed the capacity of our mental health services, translating to long wait times and deteriorating mental health during this wait (Royal College of Psychiatrists, 2022; Trades Union Congress, 2018). This is particularly concerning with possible funding cuts for mental health treatments on the horizon (The Guardian, 2022), though transdiagnostic treatments may offer a solution. Mental health practitioners would require training in a single transdiagnostic treatment that could enable them to treat a range of mental health disorders, translating to a range of benefits for service users and providers alike. For instance, quicker, cheaper, and more resourceful training programs to increase the number of qualified professionals, translating into greater accessibility for those in need of treatment.
The meta-analysis conducted by Hogg and colleagues offers one such focus for transdiagnostic treatment: trauma exposure. While every individual presenting to mental health services with a psychiatric disorder certainly won’t have been exposed to trauma, symptoms in individuals that have been exposed to trauma may be driven by trauma-related mechanisms. It is therefore important that treatment address these mechanisms, and if they are shared across disorders, it is a perfect example of when transdiagnostic treatment may be beneficial. Further research would certainly be needed to identify and explore the range of mechanisms linking trauma exposure and mental health outcomes that could be targeted during treatment, but the described study certainly provides grounds for optimism moving forward.

With the demand for mental health services far exceeding capacity, a transdiagnostic treatment targeting trauma-related mechanisms would enable more resourceful training programs for service providers, increasing accessibility.
Statement of interests
None.
Links
Primary paper
Hogg, B., Gardoki-Souto, I., Valiente-Gómez, A., Rosa, A. R., Fortea, L., Radua, J., Amann, B. L., & Moreno-Alcázar, A. (2022). Psychological trauma as a transdiagnostic risk factor for mental disorder: an umbrella meta-analysis. European Archives of Psychiatry and Clinical Neuroscience, 1-14.
Other references
Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., Shahly, V., Stein, D. J., Petukhova, M., Hill, E., Alonso, J., Atwoli, L., Bunting, B., Bruffaerts, R., Caldas-de-Almeida, J. M., de Girolamo, G., Florescu, S., Gureje, O., Huang, Y., . . . Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327-343.
Borsboom, D., Cramer, A. O. J., Schmittmann, V. D., Epskamp, S., & Waldorp, L. J. (2011). The Small World of Psychopathology. PLOS ONE, 6(11), e27407.
Campbell, D. (2022, October 6). NHS England could face £7bn budget shortfall next year, finance chief warns. The Guardian.
Fusar‐Poli, P. (2019). TRANSD recommendations: improving transdiagnostic research in psychiatry. World Psychiatry, 18(3), 361-362.
Green, J. G., McLaughlin, K. A., Berglund, P. A., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2010). Childhood Adversities and Adult Psychiatric Disorders in the National Comorbidity Survey Replication I: Associations With First Onset of DSM-IV Disorders. Archives of General Psychiatry, 67(2), 113-123.
Huang, L. N., Flatow, R., Biggs, T., Afayee, S., Smith, K., Clark, T., & Blake, M. (2014). SAMHSA’s Concept of Trauma and Guidance for a Trauma- Informed Approach. HHS Publication No. (SMA) 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Ioannidis, J. P. (2009). Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. Canadian Medical Association Journal, 181(8), 488-493.
Kessler, R. C., McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., Aguilar-Gaxiola, S., Alhamzawi, A. O., Alonso, J., Angermeyer, M., Benjet, C., Bromet, E., Chatterji, S., de Girolamo, G., Demyttenaere, K., Fayyad, J., Florescu, S., Gal, G., Gureje, O., . . . Williams, D. R. (2010). Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. British Journal of Psychiatry, 197(5), 378-385.
McLaughlin, K. A., Greif Green, J., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2012). Childhood Adversities and First Onset of Psychiatric Disorders in a National Sample of US Adolescents. Archives of General Psychiatry, 69(11), 1151-1160.
Royal College of Psychiatrists (2022, October 10). Hidden waits force more than three quarters of mental health patients to seek help from emergency services [Press release].
Shea, B. J., Grimshaw, J. M., Wells, G. A., Boers, M., Andersson, N., Hamel, C., Porter, A. C., Tugwell, P., Moher, D., & Bouter, L. M. (2007). Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology, 7(1), 10.
Trades Union Congress (2018, October 19). Breaking point: the crisis in mental health funding.
Photo credits
Source link
#Trauma #transdiagnostic #risk #mental #health

