Cancer Research UK – Science blog
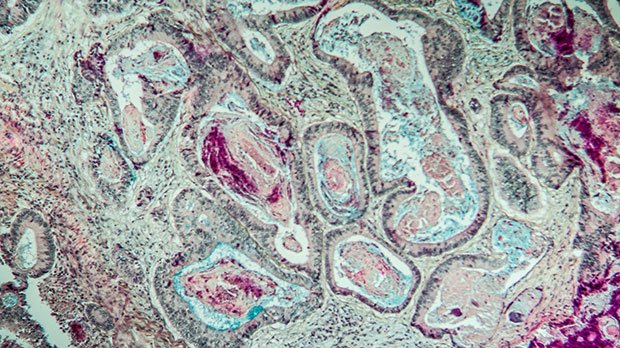
Bowel cancer cells under the microscope
After a new treatment has been developed in the lab, it has to be rigorously tested in a clinical trial before it can be used widely in patients.
Through a clinical trial, researchers can test whether a new treatment is safe, has any side effects, is better than existing treatments, or affects quality of life.
Just like with every area of cancer research, researchers are constantly working to improve clinical trials, implementing new, ambitious trial designs to make them as effective and efficient as possible.
And when a trial comes to an end, it presents an opportunity to reflect on its successes and areas for improvement.
FOCUS4 was a large-scale, multi-arm multi-stage, randomised trial investigating a range of new treatments in people newly diagnosed with advanced or metastatic colorectal cancer.
Funded by us and the Efficacy and Mechanism Evaluation Programme, a partnership between the Medical Research Council (MRC) and the National Institute for Health and Care Research, the trial ran for almost 7 years, starting to recruit participants in January 2014 and closing in October 2020.
One of the first clinical trials of its kind, FOCUS4 was what’s called a stratified, adaptive trial. It was both a trial of treatments for colorectal cancer, and a trial of its own methodology, one that hadn’t been done in colorectal cancer before, or any solid tumours for that matter.
Though stratified trials are becoming more common, back in 2011 when FOCUS4 was conceived by the NCRI Colorectal Group, they were still relatively novel, particularly on the scale FOCUS4 was aiming for.
But before we dive into the specifics of FOCUS4, let’s answer a question you might have on your mind.
What’s a stratified trial?
Luckily, it’s not quite as complicated as it might sound. So, let’s break it down.
Cancers are caused by mutations, small changes to our DNA that accumulate over time and can result in uncontrolled replication of cells – the growth of a tumour. Some mutations that cause cancers to begin are random, and a cancer may start growing simply because a cell has acquired one too many for it to function normally.
However, mutations in some genes are associated with an increased likelihood of developing particular types of cancer. For example, a mutation in a gene called EGFR that causes it to make too much of a particular protein, also called EGFR, is associated with lung cancers.
But because we know about these relationships, we have specific drugs that target these mutations, often counteracting the effect that the mutation has on a cell. To continue the previous example, drugs like erlotinib and gefitinib both inhibit the activity of the EGFR protein, which slows down cancer growth.
That means if we can analyse a sample of a person’s tumour and identify what mutations appear in its DNA, we can try to match these people with a drug that might be more effective in treating it.
Therefore, if a new drug is developed that targets cancers with certain mutations, we can analyse the tumour of patients to make sure they have that mutation before they’re accepted onto the trial to test it.
And we can do this for multiple drugs within the same trial, matching patients with different mutations to different drugs that need testing in separate trial arms that run concurrently.
In short, running a stratified trial is like running multiple smaller trials at once, all under the header of one big trial.
What about adaptive?
The adaptive part means that trial arms can be opened or closed reactively throughout the course of the trial.
For example, if a trial runs three groups each testing a different drug on a different mutation, but midway through the trial it’s obvious that one of these drugs is having no effect, that arm of the trial can be closed early, and patients can be reassigned to a different trial arm if appropriate.
On the flipside, if while the trial is running a fourth drug is developed that needs testing, a new arm can be opened to allow for that to happen in parallel with the others. Similarly, if new science suggests another type of mutation might be responsive to a drug already being tested, the trial can broaden the eligibility criteria to include the new mutation.
Making the trial design adaptive means we can make sure time and resources are being used more effectively. By closing a trial arm that might not be working, we can free up space for the testing of another drug should it come along.
And if that weren’t enough, FOCUS4 also used what’s called a seamless design in relation to the phase of the clinical trial.
Usually, new treatments would go through several clinical trials sequentially, from phase 1, which broadly tests a drug’s safety and works out the correct dosage, through phase 2 to see if the drug demonstrates promise in a small, tightly controlled trial, to phase 3, testing its efficacy against the current standard of care.
In FOCUS4, the trial was designed to move seamlessly from phase 2 into phase 3 if a drug was showing early promise of benefit, continuing recruitment into phase 3 while retaining the patients already enrolled.
Seamless design trials are more efficient, avoiding the time and costs involved in setting up multiple back-to-back trials.
So, those are the basic principles of the trial design. Let’s get into what FOCUS4 did.
The procedure
“Patients who are stable and responding to their first line chemotherapy in the UK would typically be considered for a treatment break,” says Professor Louise Brown, who was project lead of FOCUS4.
“Previous work we’ve done has demonstrated that it’s safe, in terms of overall survival, to give people a break, and just monitor their tumour so that if it shows signs of coming back, you can immediately restart that first line chemotherapy.
“But that also opened up an opportunity for us to say, ‘in that treatment break, let’s see if we can test new drugs.’”
To do that, FOCUS4 ran three stratified trial arms, called B, C and D, each testing one drug in patients with certain mutations after the standard 16 weeks of chemotherapy when patients would be starting a treatment break.
They were measuring what’s called progression-free survival (PFS), meaning how long a patient lives before their cancer gets bigger.
- FOCUS4-B tested aspirin in people with a mutation in a gene called PIK3CA
- FOCUS4-C tested a drug called adavosertib, a Wee1 inhibitor, in people with mutations in the RAS and P53 genes
- FOCUS4-D tested a drug called AZD8931, a tyrosine kinase inhibitor, in people with none of the above mutations, but who did express a protein called PTEN
But it also ran one non-stratified arm, FOCUS4-N.
“As it turned out, the non-stratified arm was one of the most important parts of the design,” Brown explains. “As most people won’t necessarily have the molecular subtype of interest.”
“We felt it would have been very unfortunate for patients to have given their tissue for testing, and then they don’t have the ‘right’ kind of cancer to go into a trial. So, we thought it was important to offer them a clinical trial to answer another, more generic research question.”
FOCUS4-N investigated whether continuing chemotherapy with a drug called capecitabine improved PFS compared to patients who were given no treatment but actively monitored.
The findings
As could be expected with trialling a new method, it wasn’t totally smooth sailing. Two of the four trial arms were closed early, but for different reasons.
FOCUS4-B was closed early due to low patient recruitment; not enough patients that submitted their tissue for testing had the necessary mutation, but mainly because asking a patient to take a placebo drug in this setting is particularly challenging.
As aspirin is readily available over the counter at pharmacies, some patients decided to just take the aspirin in case it helped.
But the closure of FOCUS4-D is actually a perfect example of how an adaptive trial design can be beneficial.
“We were able to make a very clear decision to discontinue arm D after 32 patients,” says Professor Tim Maughan, chief investigator of the trial.
“And the reason we were able to be so clear about that was because it was a randomised trial.”
In a randomised trial, patients are randomly assigned to either receive the drug being investigated, or a placebo, to allow for a direct comparison of the effect of the drug.
After the trial arm had been open for a prespecified amount of time, an independent monitoring committee reviewed the data and determined that AZD8931 wasn’t having enough of an impact compared to the placebo for the trial arm to continue.
But in another trial arm, FOCUS4-C, the randomisation allowed the researchers to see the opposite. Adavosertib was improving PFS vs the active monitoring alone in patients with mutations in RAS and P53 genes, extending it by around 2 months on average.
“We used the combination of KRAS mutation and P53 mutation,” Maughan says.
“One of the things we’ve learned from it is that that double mutation does define a group of quite poor prognosis. And clearly, the Wee1 inhibitor was doing something.”
Having identified that this Wee1 inhibitor was showing efficacy, the team are now working to design a follow-up trial to test it in what’s called the third-line setting, meaning when initial and subsequent therapies have stopped working, to bring this type of drug to the clinic as soon as possible.
The reflections
It’s still relatively early days since the results of FOCUS4 were published in 2021, but both the positive and negative results bring us one step closer to finding new treatments for metastatic colorectal cancer.
We have a new potential biomarker to explore as a target and know that some drugs aren’t effective when targeting certain biomarkers and we can stop investigating them.
But on top of the papers the team published detailing the results of each trial arm, they also published a paper after gathering feedback from those involved in the trial, reflecting on its successes and where the trial design didn’t work as well as intended.
“We were testing this new design, and therefore, we felt to close the loop on that work we should understand how it worked across all the people who were involved,” Brown says. “That way, we could try and learn and maybe do things better or differently in future ventures.”
Publishing learnings in this way isn’t common in clinical trials but gives us vital insight into how we can improve clinical trials, especially those of this scale, in the future.
So, what did we learn?
The learnings
For starters, at the core of a trial like this, is you need to ensure you have sufficient resource.
“These sorts of trials are really efficient in that they answer lots of questions at the same time,” says Brown.
“They bring the timelines in, and you get an answer sooner, rather than doing them all as separate trials, but they probably don’t necessarily save a great deal of resource.”
“We thought that there would be efficiencies in building the infrastructure. And therefore, we suspected there’d be a lot less work for each of the sub trials.
“But as it turned out, each sub trial is still a whole trial in its own right. And you need people, trial managers and data managers to do that, to make sure that you’re ticking all the right boxes and not putting patients at harm.”
Luckily, FOCUS4 was run from exactly the right place to overcome these challenges.
“We were running the trial in the MRC Clinical Trials Unit. I don’t think we could have done this trial in another, smaller unit, because we had to often draw upon other staff within the unit temporarily when times were particularly busy.
“You can’t just put a job advert out; you need a pool of staff that you can draw on during times of particularly intensive workload.”
Making connections
For a trial like this, where you’re testing new drugs coming out of development, it’s about building relationships.
“You’ve got to have multiple different biomarkers for the different cohorts, and need different drugs for each of the different subgroups,” Maughan explains.
“And you really need to have major pharma involvement to give you the range of potential pharmaceuticals that might be relevant.”
This isn’t such a problem in a kind of stratified trial called a basket trial, where you identify one mutation in several cancer types and test one drug in all of them, as it only requires one new drug. But FOCUS4 was an umbrella trial, looking at several different mutations within the same cancer type.
This required working with multiple pharma companies within the same trial, which can be challenging.
And unfortunately for FOCUS4, the range of drugs they expected to become available to test over the course of the trial didn’t materialise.
“We thought there were going to be lots of new drug opportunities to slot into this design and test,” says Brown. “But as it turned out, a lot of them just failed at the end of the phase 1 and never made it to the phase 2 setting.”
However, if FOCUS4 were to run again, that may not be such a problem. That’s because since then, our understanding of, and ability to identify, biomarkers in tumours that may act as potential drug targets has greatly improved, and with that has come several new research projects that may have given FOCUS4 a helping hand.
Building a network
The first of those is S:CORT, a multidisciplinary group of nationwide researchers led by Maughan.
S:CORT is performing detailed molecular analysis of tumour samples and correlating the results with clinical outcomes of treatment with the aim of being able to better predict patient response to treatment.
In doing this, S:CORT has shown that there are factors beyond the genetic changes in a tumour that determine how it responds to treatment. For example, how the patient’s immune system responds to the cancer has an effect and can even protect the cancer from the effects of therapy.
By understanding cancer at both the genetic and host response levels, we can offer treatments in a more targeted manner, thereby sparing people from treatments that are less likely to be successful.
The second is ACRCelerate, led by Professor Owen Sansom in Glasgow, a consortium of scientists across Europe at the forefront of colorectal cancer research, partly funded by us.
ACRCelerate identifies new drug targets amongst the DNA signatures picked up by S:CORT and accelerating the development of drugs to target them.
And these groups can work together, and even feed into one another. S:CORT can identify DNA signatures that we can use to stratify patients, ACRCelerate can take these signatures and identify new potential drug targets, and that can feed into a stratified trial where we can test new agents targeting these signatures.
Were groups like these around when FOCUS4 began, it may have had a healthier pipeline of new drugs to slot into its design, opening new arms that recruited patients with different mutations.
It may be that FOCUS4 was a small step ahead of its time, trialling new ideas when the clinical trials landscape wasn’t quite ready for it, but we have learned a great deal from it.
The future of stratified trials
Running FOCUS4 may not have been without its challenges, but the learnings it provided us with are invaluable if we’re to run trials like it again.
“Was it the best way to do it? It’s certainly a challenging way to do it,” Maughan reflects.
“If you’ve got the buy in from pharma, and if you’ve got relatively simple biomarkers, then it remains a viable and efficient option. But you do need to have those features.”
Clinical trials are the cornerstone of drug development, and without them, we couldn’t bring new treatments from lab bench to bedside, but a ‘successful’ trial may not always mean one that produces a new treatment as quickly as possible.
Trials that show that a new treatment is having no effect, has severe side effects, or that has little or no additional benefit than the current standard of care all provide us with vital information we can use to improve the safety and efficacy of cancer treatment.
And if we continue to collect, and importantly publish, learnings from these large-scale trials, as the FOCUS4 team did, we can continue to refine them, bringing the benefits of the data we gather to patients sooner.
Jacob
Source link
#Cancer #Research #Science #blog



